- Truveta and collaborators partnered on a new large-scale study that considers the potential benefits of GLP-1 RA for AUD, among those with diabetes and/or obesity.
- Using a target trial emulation framework, researchers analyzed Truveta Data and compared adults with alcohol use disorder (AUD) and either type 2 diabetes or obesity who started a newer GLP-1 RA (semaglutide, tirzepatide) to similar individuals starting alternative medications.
- The study found that newer GLP-1 RAs were associated with reduced risk of alcohol-related hospitalization across clinically distinct populations.
A new large-scale study from Truveta and collaborators from Providence, Johns Hopkins, Duke University, and more suggests that glucagon-like peptide-1 receptor agonists (GLP-1 RAs)—semaglutide and tirzepatide—may have another powerful benefit: reducing alcohol-related hospitalizations in people with alcohol use disorder (AUD).
Alcohol use disorder affects around 10% of adults in the United States, yet only 2% receive medications approved for AUD (MAUD), and among those who do, medication adherence is often poor. This study considers the potential benefits of GLP-1 RA for AUD, among those with diabetes and/or obesity.
Researchers used Truveta Data from over 40,000 patients to assess whether newer GLP-1 RA medications – semaglutide and tirzepatide, commonly known by brand names Ozempic, Wegovy, Mounjaro, and Zepbound – are associated with lower risks of emergency department visits and hospitalizations related to alcohol use.
Study design: Real-world data, real impact
Using a target trial emulation framework, researchers analyzed Truveta Data and compared adults with AUD and either type 2 diabetes or obesity who started a GLP-1 RA to similar individuals starting alternative medications.
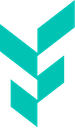
They ran four parallel studies based on different patient profiles:
- ADM trial: Patients with type 2 diabetes (T2D), comparing newer GLP-1 RAs to older GLP-1 RAs, sulfonylureas, and other anti-diabetic medications (ADMs).
- AOM trial: Patients with obesity but without T2D, comparing newer GLP-1 RAs to older GLP-1 RAs and other anti-obesity medications (AOMs).
- MAUD-T2D trial: Patients with T2D and markers of more severe AUD, comparing newer GLP-1 RAs to FDA-approved medications for AUD (MAUD: acamprosate, disulfiram, or naltrexone).
- MAUD-obesity trial: Patients with obesity, no T2D, and markers of more severe AUD, comparing newer GLP-1 RAs to MAUD.
All studies used balanced populations (inverse probability of treatment weighting or propensity score matching) and accounted for informative censoring (inverse probability of censoring weighting).
Key findings
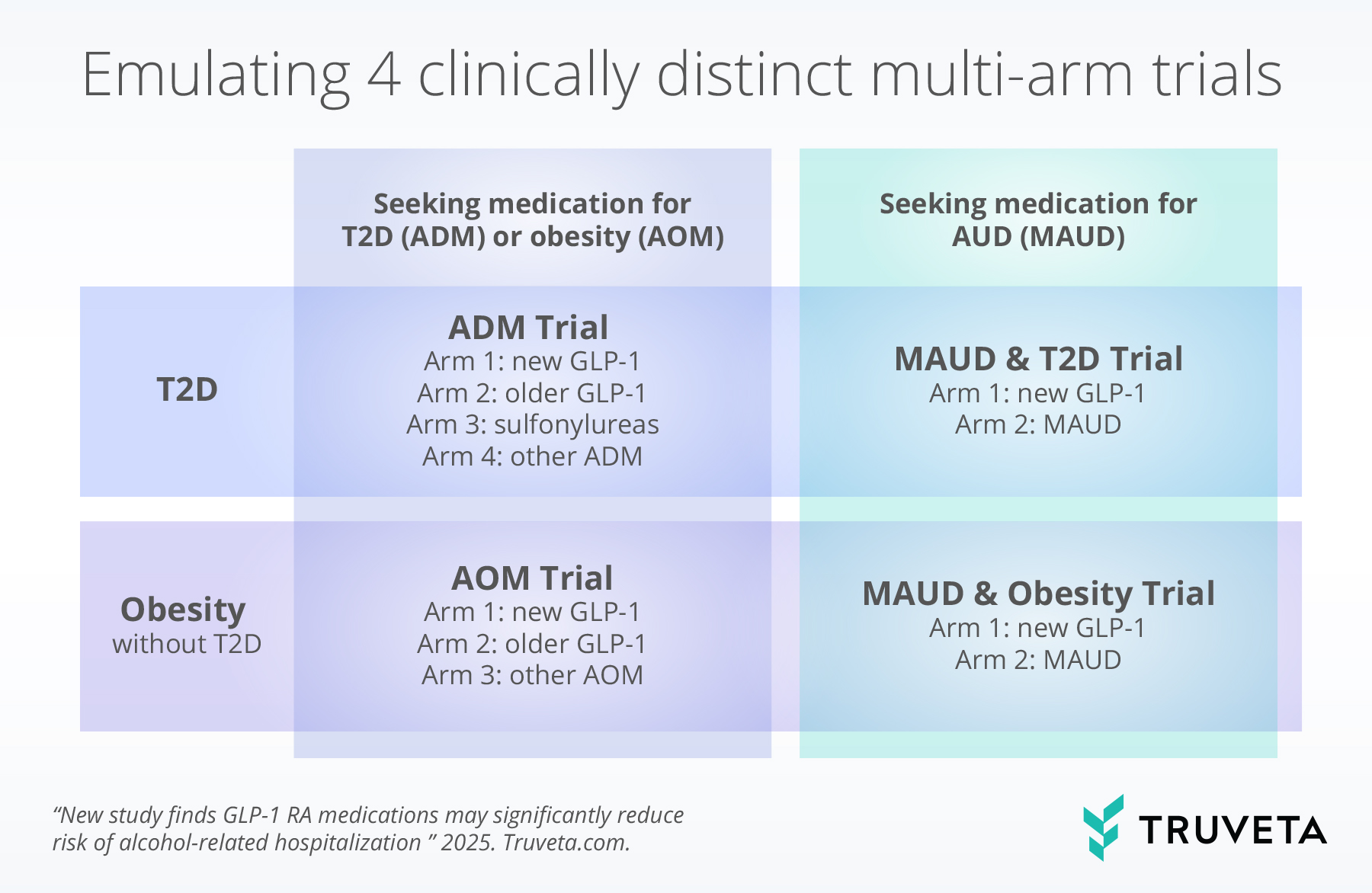
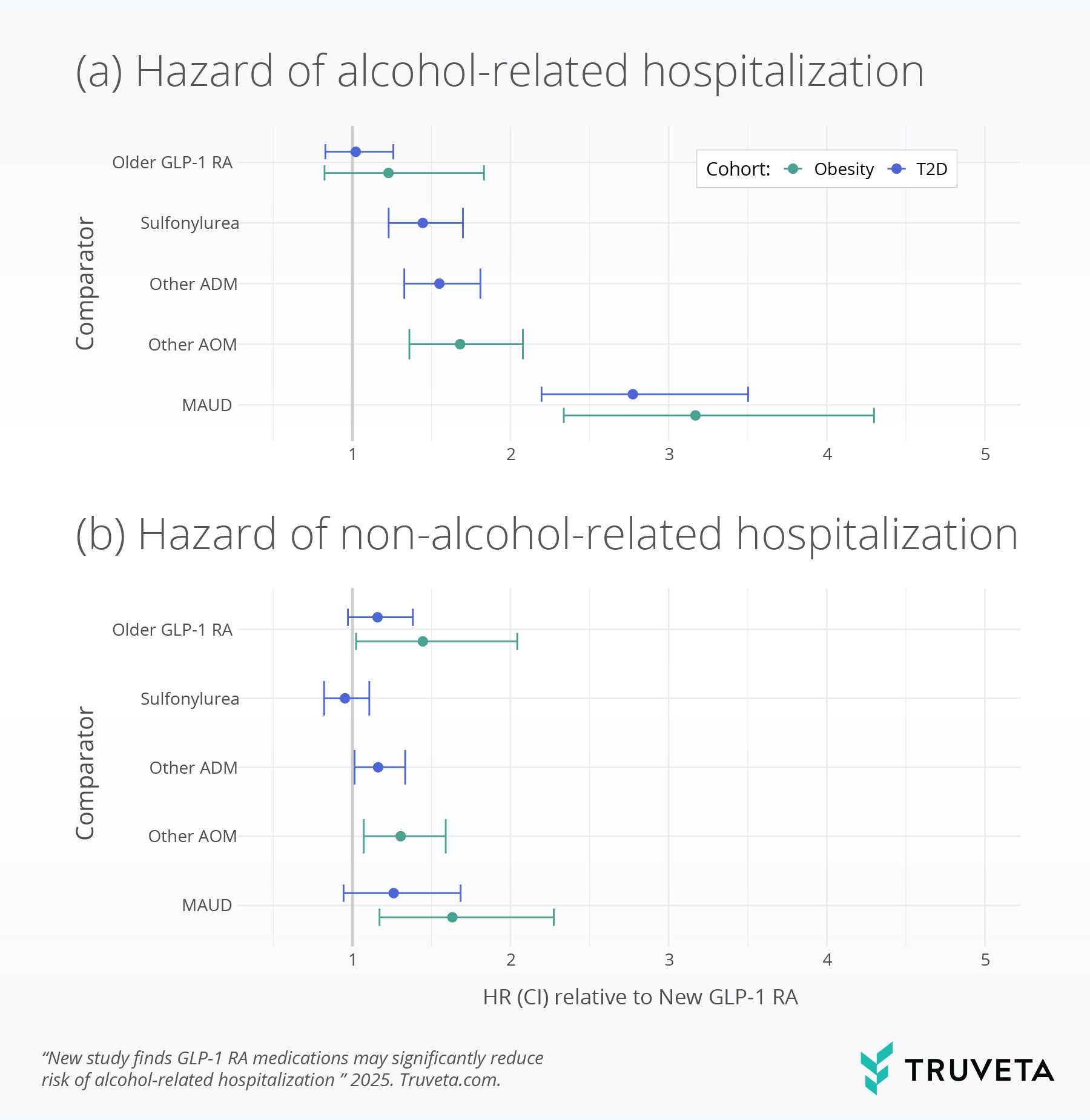
Across all four trials, GLP-1 RAs were consistently associated with lower rates of alcohol-related hospitalization within one year in balanced populations:
- ADM trial (n = 18,515): Alcohol-related hospitalization occurred in 10.1% of newer GLP-1 RA users vs. 14.4% of sulfonylurea users and 13.9% of other ADM users.
- AOM trial (n = 9,256): Alcohol-related hospitalization occurred in 7.5% of newer GLP-1 RA users vs. 12.1% of other AOM users.
- MAUD-T2D trial (n = 3,178): Alcohol-related hospitalization occurred in 12.9% of newer GLP-1 RA users and 31.1% of MAUD users.
- MAUD-Obesity Trial (n = 3,276): Alcohol-related hospitalization occurred in 10.2% of newer GLP-1 RA users and 28.5% of MAUD users.
Notably, researchers observed no similar reduction in hospitalizations unrelated to alcohol in T2D populations and smaller impacts on hospitalizations unrelated to alcohol in populations with obesity, suggesting the effect may be specific to alcohol-related outcomes, rather than confounding by underlying health status or general improvements in health.
All study methodology and findings are available on MedRxiv.
Why this matters
Semaglutide and tirzepatide could represent a new frontier in treating patients with alcohol use disorder—especially appealing because they are already in widespread use for other conditions and appear to be well tolerated.
While the exact mechanism is still under investigation, GLP-1 RAs may affect brain pathways involved in reward, reducing cravings and alcohol intake. Animal studies and small human trials have shown similar trends, and this new study builds additional evidence with larger and more generalizable real-world populations.
For clinicians, it opens the door to consider these medications not only for metabolic health but potentially for reducing alcohol-related harm. For patients with both AUD and conditions like diabetes or obesity, they could serve a dual purpose.