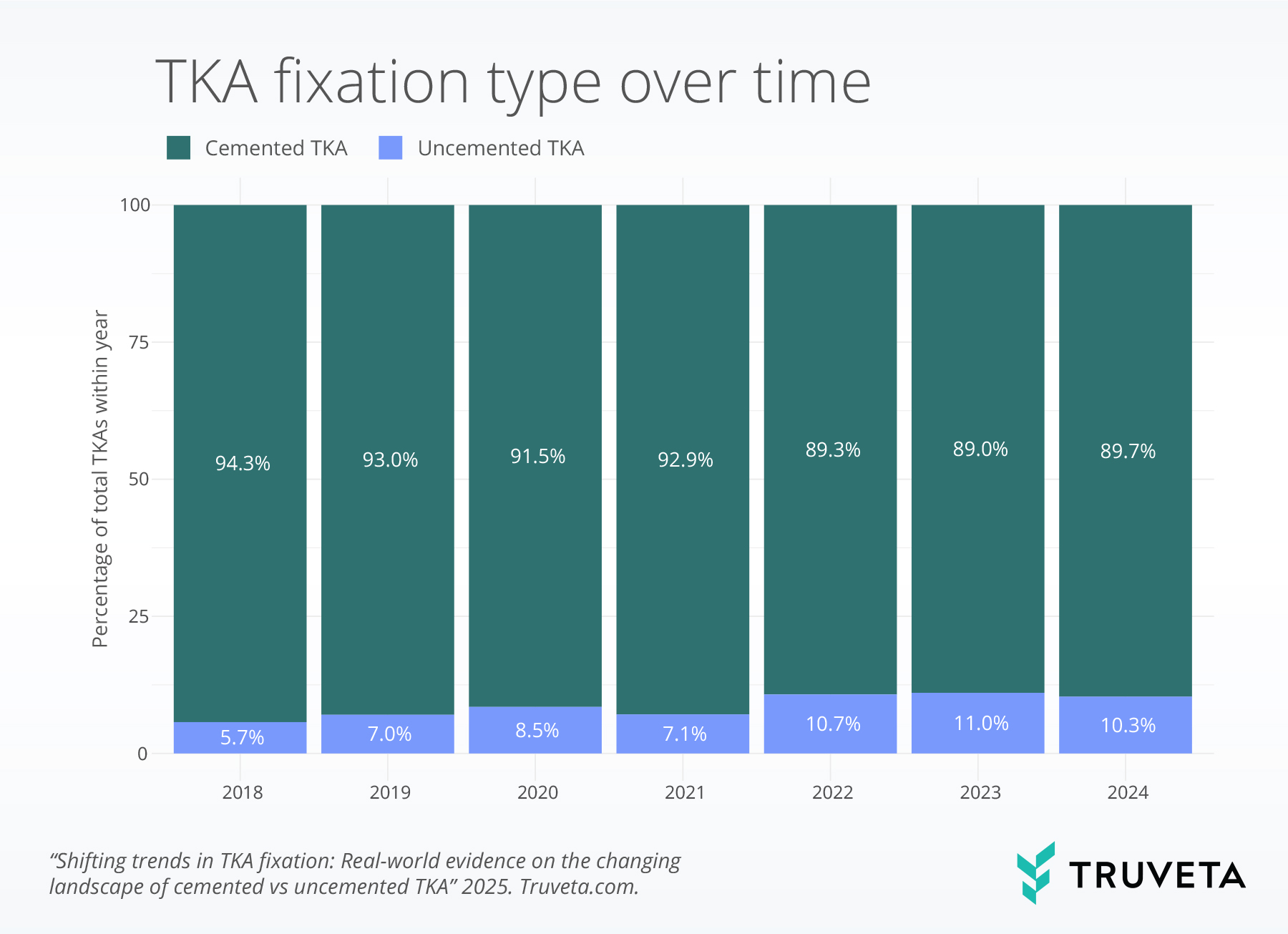
- The percentage of uncemented total knee arthroplasties (TKAs) nearly doubled from 5.7% to 10.3% between 2018 and 2024.
- Readmission and revision rates were similar between cemented and uncemented TKAs.
- Cemented TKAs were associated with higher rates of stiffness, fracture, infection, and chronic pain, even after accounting for patient age and comorbidities.
Total knee arthroplasty (TKA), commonly referred to as a total knee replacement, is a surgical procedure that replaces the knee joint with artificial components to relieve pain and restore mobility. TKAs are common for patients with osteoarthritis, rheumatoid arthritis, or osteoporosis (1, 2). A key factor influencing long-term outcomes is the method of implant fixation, with two primary approaches: cemented and uncemented fixation.
Cemented TKA uses bone cement (polymethylmethacrylate, or PMMA) to anchor the implant, providing strong initial fixation and effective force transfer between bone and prosthesis (1, 3). Uncemented TKA features roughened or porous implant surfaces that promote bone growth into the implant, creating a biological bond (4). Studies suggest that cemented TKA has lower early revision (replacement) rates and remains the preferred choice for older patients or those with weaker bone quality (5, 6). However, advancements in uncemented implants have improved fixation and may offer superior long-term durability, particularly for younger, more active patients (7). Despite these potential benefits, the choice between cemented and uncemented TKA remains debated, as uncemented implants still face concerns about higher early failure rates, periprosthetic bone loss, and aseptic loosening (8). As implant design and biomaterials continue to improve, the long-term outcomes of uncemented TKA may continue to evolve (9–12).
Understanding trends in utilization and outcomes of cemented versus uncemented TKA is key to surgical decision-making. As implant technologies evolve, incorporating device-level data becomes increasingly important for tracking performance and informing evidence-based practice. This report examines trends in fixation method use, revision rates, postoperative complications, and readmissions using a real-world dataset. You can also view the report directly in Truveta Studio.
Methods
Using a subset of Truveta Data, we included adults aged 45 and older who had received a TKA in an inpatient setting between January 2018 and March 2025. We used ICD-10-PCS to distinguish between cemented and uncemented implants—an important detail not captured by CPT codes. ICD-10-PCS codes are only used in inpatient settings, and therefore, we required all patients to receive a TKA in the inpatient setting. When examining trends in cemented vs. uncemented TKAs over time, we limited the analysis to procedures occurring through 2024 to ensure a complete year-to-year comparison. We also identified individuals in the study population who received a revision TKA six months to two years after their primary TKA (defined using CPT, ICD-10-PCS, and SNOMED-CT codes).
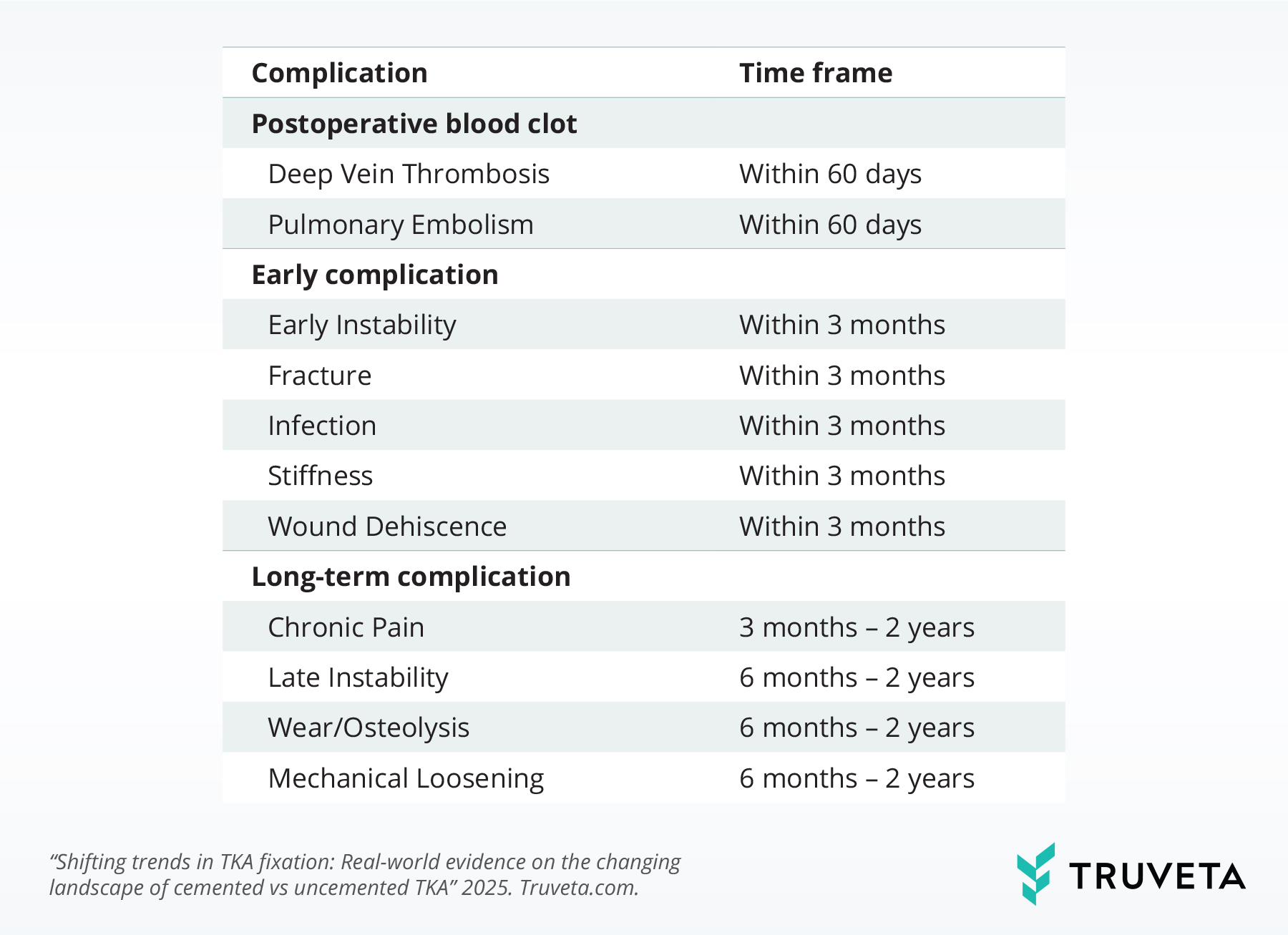
Additionally, we identified individuals who were readmitted to the hospital within 30 and 90 days after their primary TKA, and as well as those who experienced postoperative complications. Each complication was assessed within a clinically relevant time frame based on typical presentation and diagnostic patterns, as outlined below (13–19). To ensure adequate follow-up time, patients were only included in a given complication analysis if their TKA occurred prior to the required follow-up period. For example, when evaluating complications that typically occur between six months and two years after surgery, we excluded individuals who had their TKA less than two years before the end of the study period.
We used a logistic regression to see whether readmission rates, postoperative complications, and revision rates were different depending on the type of TKA a patient received. We adjusted for factors like age, BMI, and clinical history, because younger, healthier patients are more likely to receive an uncemented TKA. This allowed us to understand whether differences in outcomes were due to the type of TKA itself, rather than for health profiles that differed between patients.
When describing the results, we use the term significantly only for differences that were statistically different after accounting for patient characteristics. When rates between cemented and uncemented TKA were not statistically different after accounting for patient characteristics, we describe them as comparable or similar. We also looked at whether patient’s age changed the relationship between TKA type and the outcomes study.
Results
We identified 118,366 patients who received a primary TKA between January 2018 and March 2025. The population was 88.3% white, 7.2% Black, and 1.5% Asian. The majority of the population was female (61.0%) and was between the ages of 60-74 (55.5%). 92.2% of patients received a cemented TKA, and 7.8% of patients received an uncemented TKA.
TKA type over time
From 2018 to 2024, the rate of uncemented prostheses nearly doubled, rising from 5.7% to 10.3%—an 81.2% relative increase. This shift reflects a gradual but notable increase in adoption of uncemented fixation.
Patient demographics by TKA type
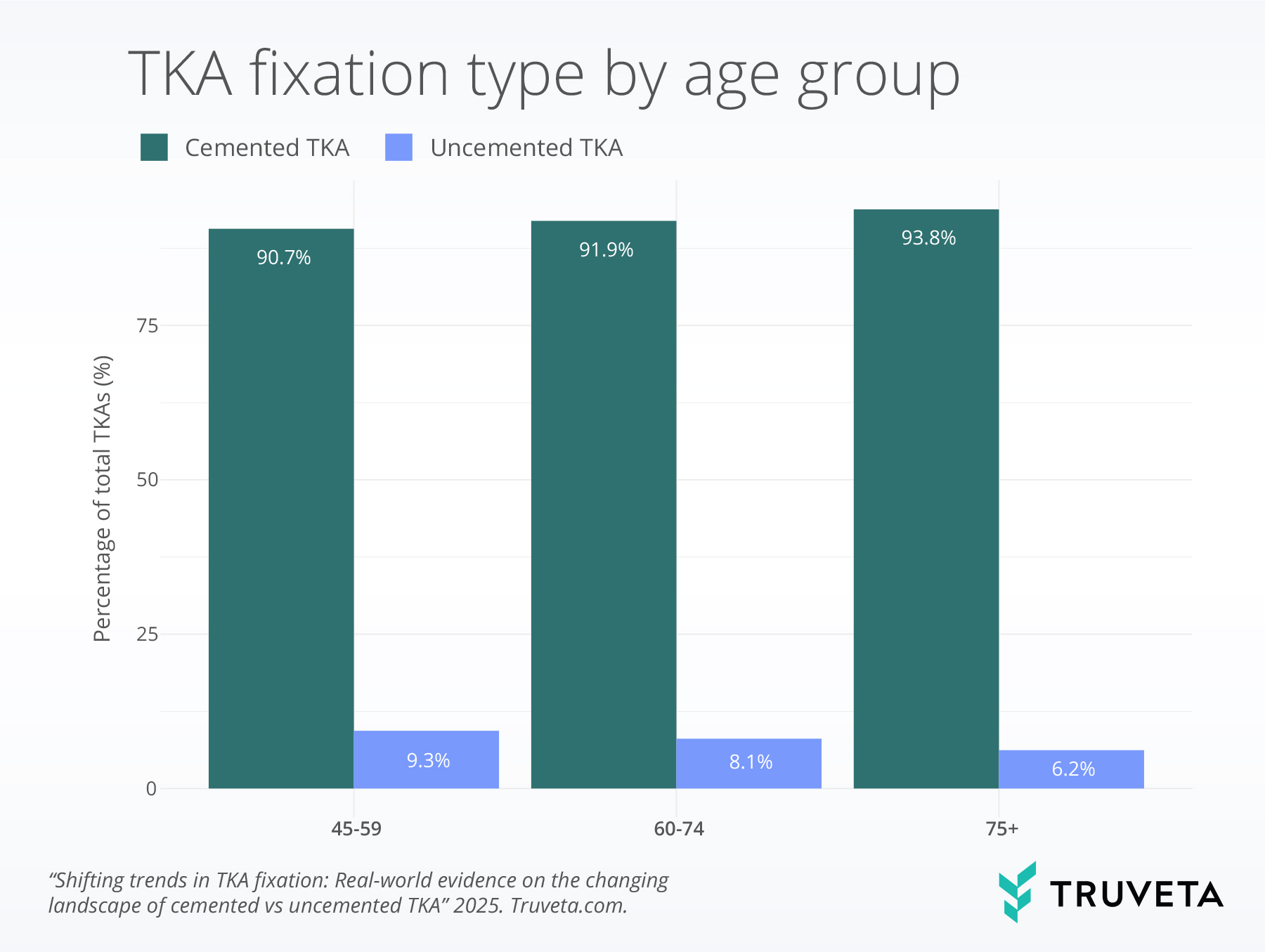
Patients who received uncemented TKAs tended to be younger. Among patients aged 45–49, 9.3% received uncemented TKAs, while only 6.2% of patients over the age of 75 received uncemented TKAs patients.
Uncemented TKAs were also more common among male patients than female patients (9.0% vs. 7.0%) and Black patients compared to white patients (10.0% vs. 7.5%).
Clinically, patients who received uncemented TKAs had lower rates of osteoporosis (4.1% vs. 7.4%), rheumatoid arthritis (5.0% vs. 8.1%), hypertension (41.3% vs. 50.5%), hyperlipidemia (34.4% vs. 43.3%), and peripheral vascular disease (23.1% vs. 31.7%), reflecting patients who received uncemented TKAs to generally be a younger and healthier population than those who received cemented TKAs.
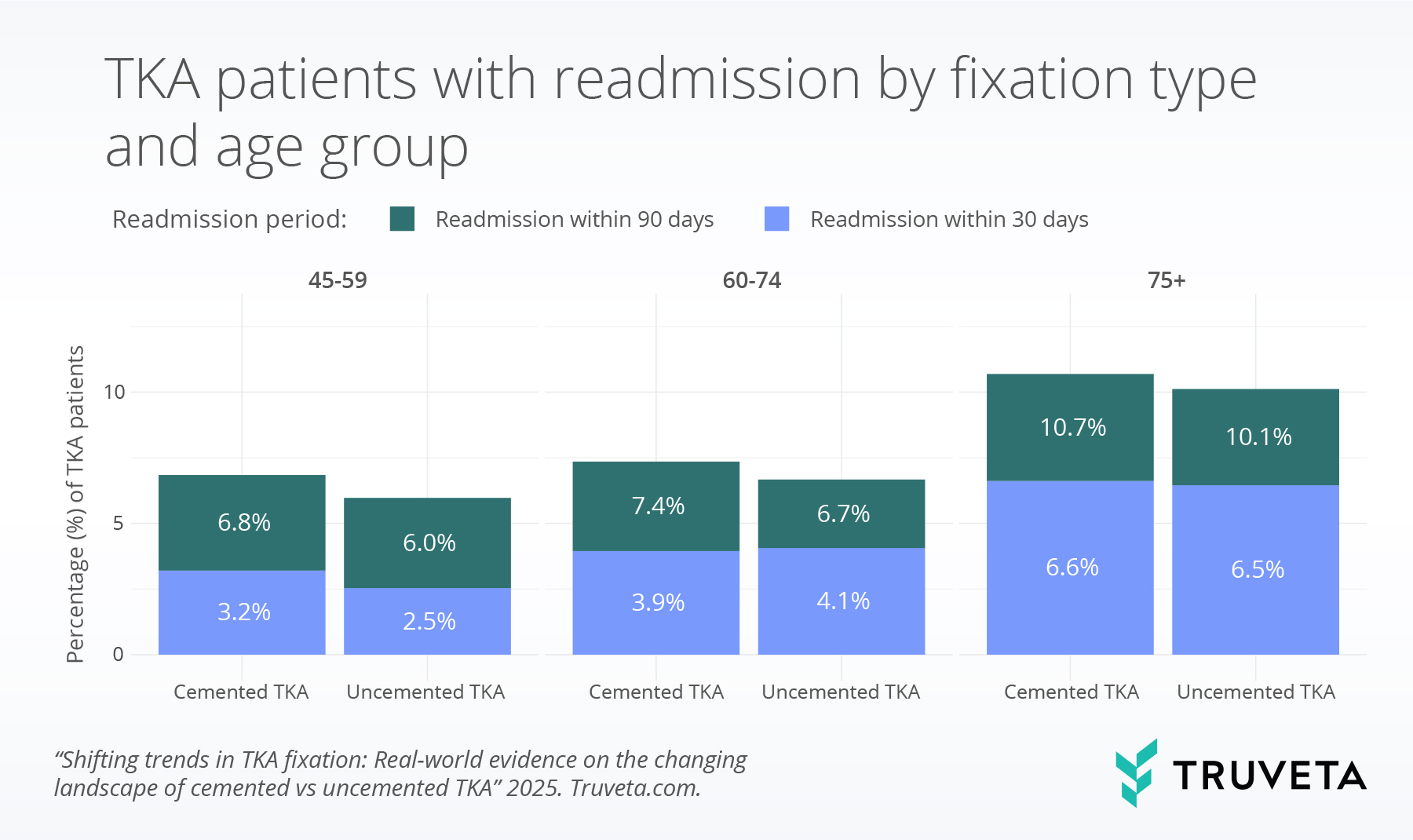
Readmission by TKA type
Overall, patients who received a cemented TKA had comparable readmission rates to those who received an uncemented TKA across both 30-day and 90-day periods.
Specifically, the 30-day readmission rate for cemented TKA was 4.6%, while uncemented TKA also had a 4.3% rate.
For 90-day readmissions, cemented TKA had an 8.2% rate compared to 7.3% for uncemented TKA.
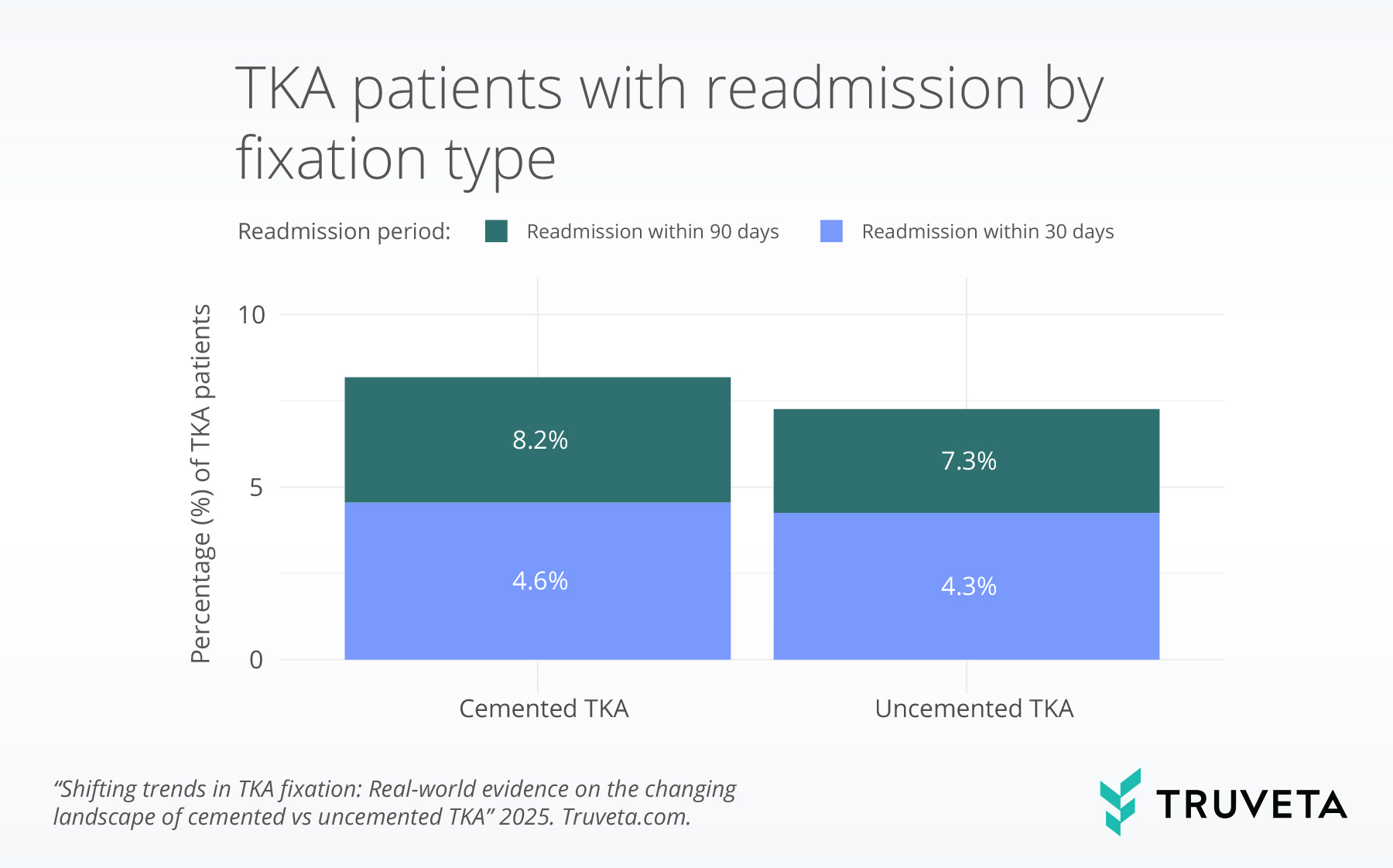
While older adults (60-74 and 75+) tended to have higher readmission rates than 45–59-year-old patients, the difference in readmission rates between cemented and uncemented TKAs did not vary significantly by age. Rates of readmission were comparable among cemented TKA patients compared to uncemented TKA patients in all age groups.
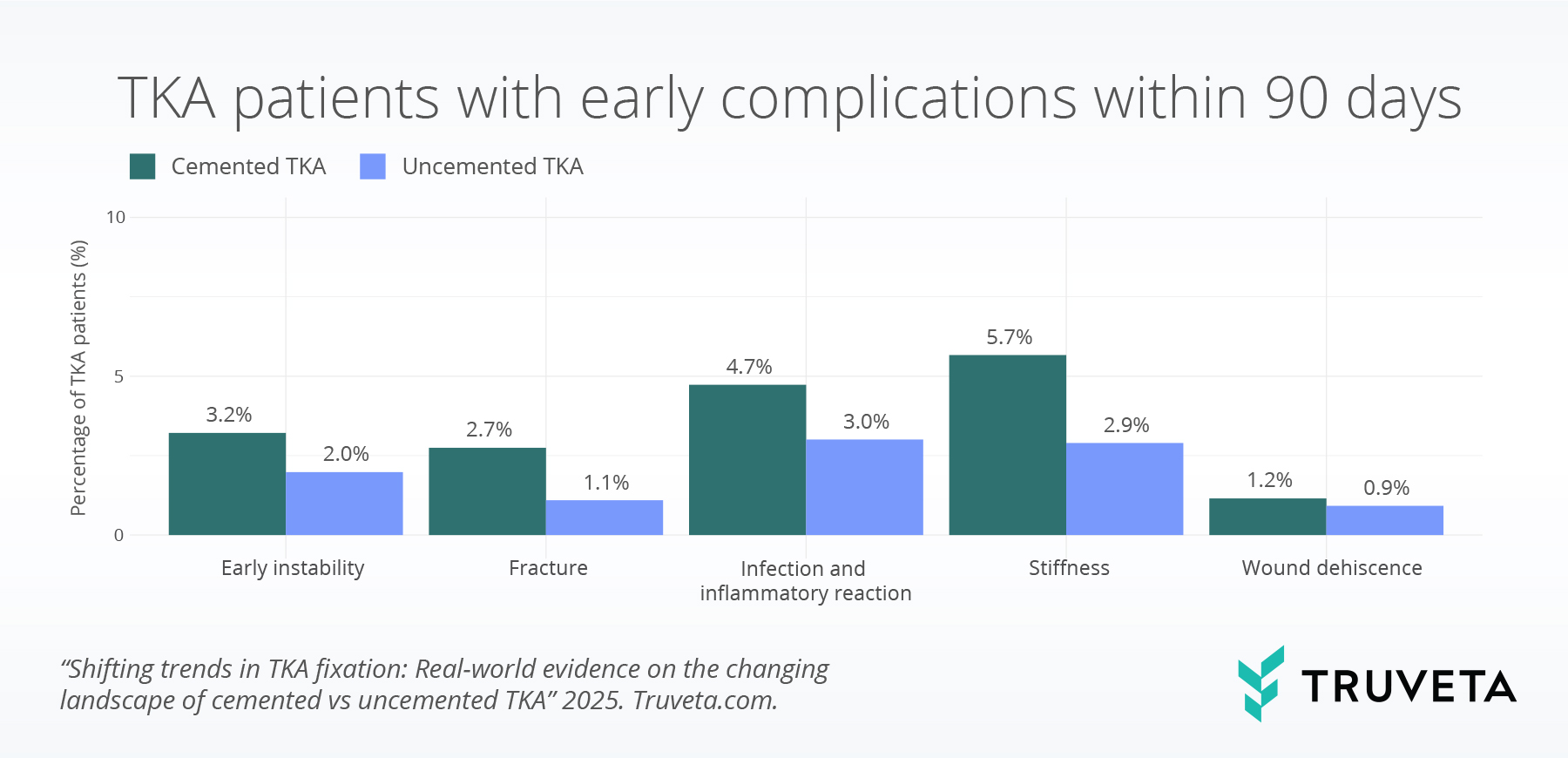
Complications by TKA type
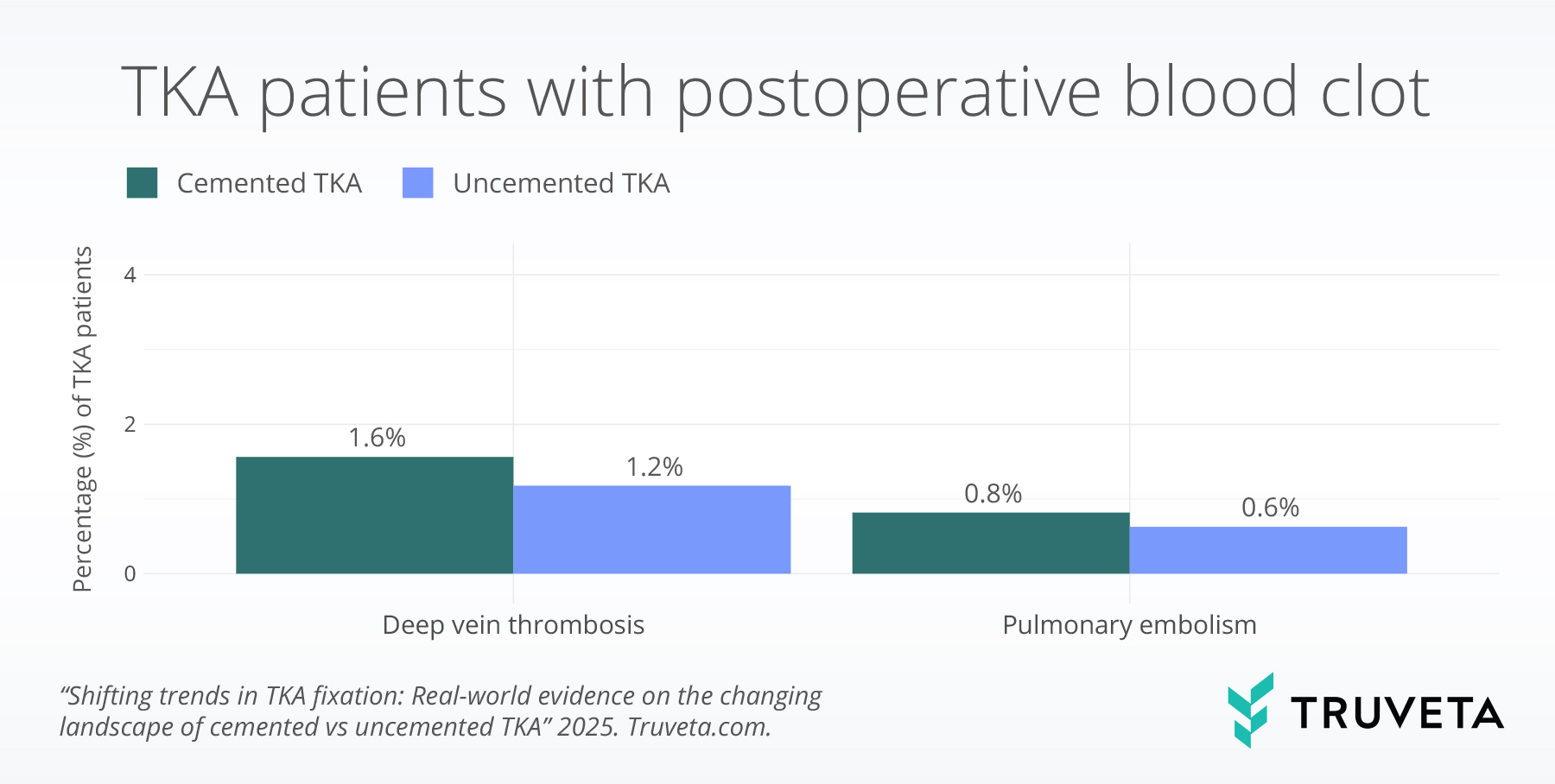
We assessed the occurrence of postoperative blood clots, including deep vein thrombosis and pulmonary embolism, following a TKA.
Overall, 1.5% of patients experienced a deep vein thrombosis, with comparable rates observed among those who received cemented (1.6%) and uncemented (1.2%) fixation.
Pulmonary embolism was less common, occurring in 0.8% of patients overall, with comparable rates between cemented (0.8%) and uncemented (0.6%) fixation. While older adults (75+) tended to have rates of postoperative blood clots, the difference between cemented and uncemented TKAs did not vary significantly by age.
Rates of early complications were significantly higher among cemented TKA patients compared to uncemented TKA patients for early instability (3.3% vs 2.0%), fracture (2.8% vs 1.1%), infection or inflammatory reaction (4.8% vs 3.0%), and stiffness (5.7% vs 2.9%).
Rates of wound dehiscence were low and comparable between fixation types.
While younger adults (45-59) had slightly higher rates of stiffness and instability complications than adults aged 60-74 and 75+, the difference between cemented and uncemented TKAs did not vary significantly by age.
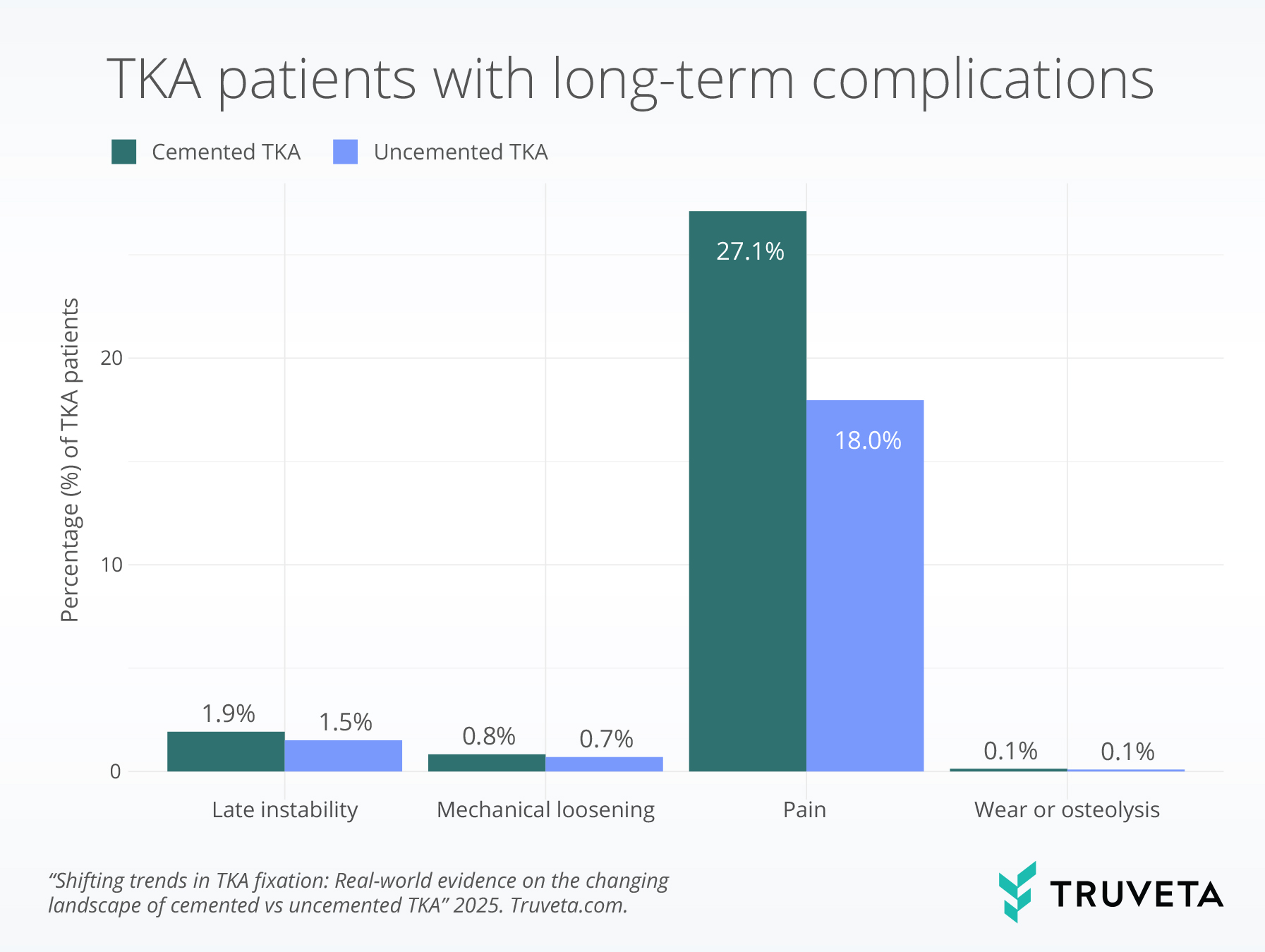
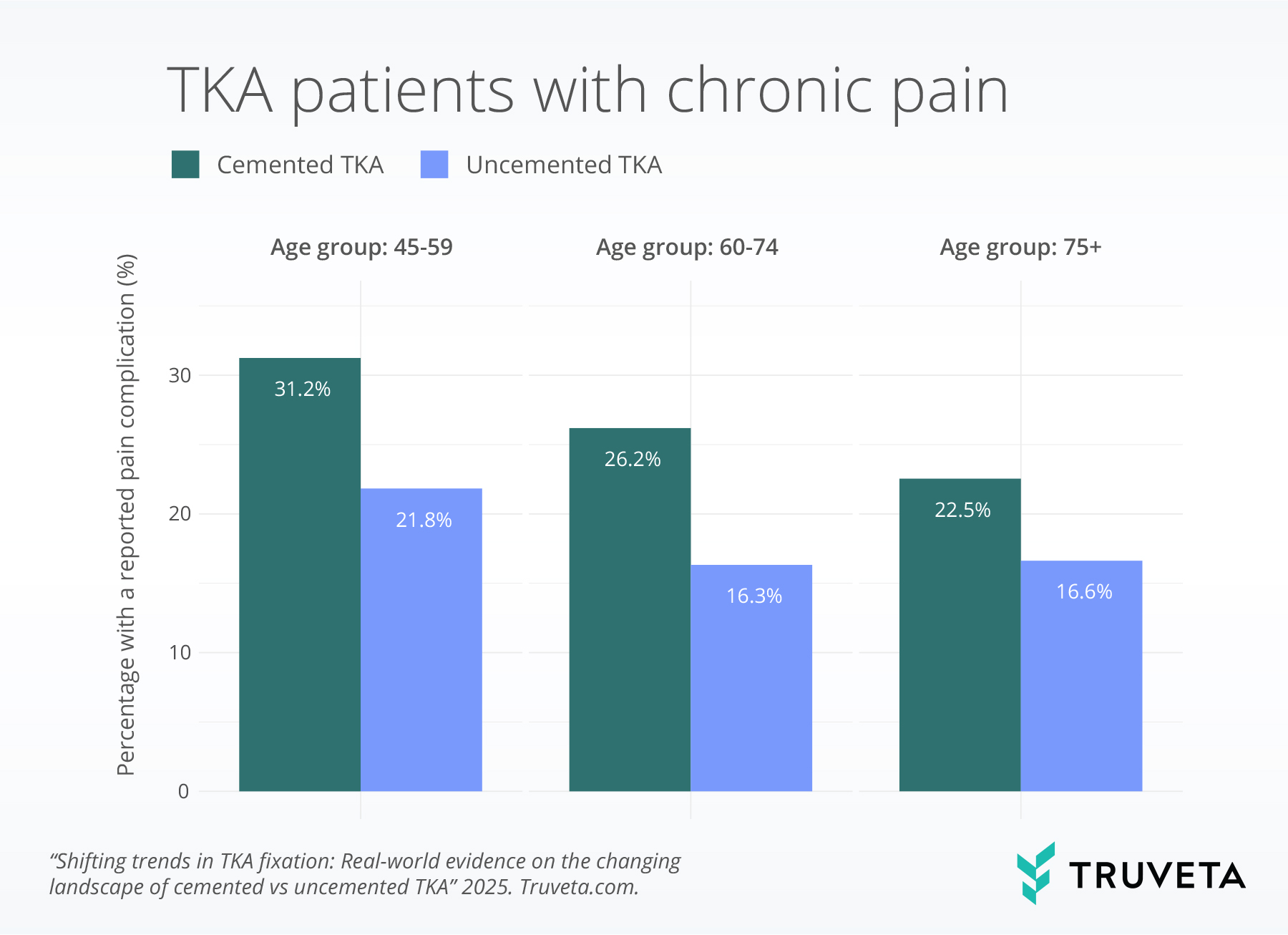
We assessed long-term complications following primary TKA, including pain, late instability, mechanical loosening, and wear of the prostheses.
Rates of pain (21.1% vs 18.0%) and late instability (1.9% vs. 1.5%) were significantly higher among patients receiving cemented TKAs compared to patients receiving uncemented TKAs.
Rates of prostheses wear/osteolysis and mechanical loosening were low and comparable between fixation methods.
While adults aged 45-59 years old tended to have higher rates of pain and mechanical loosening, the difference between cemented and uncemented TKAs did not vary significantly by age.
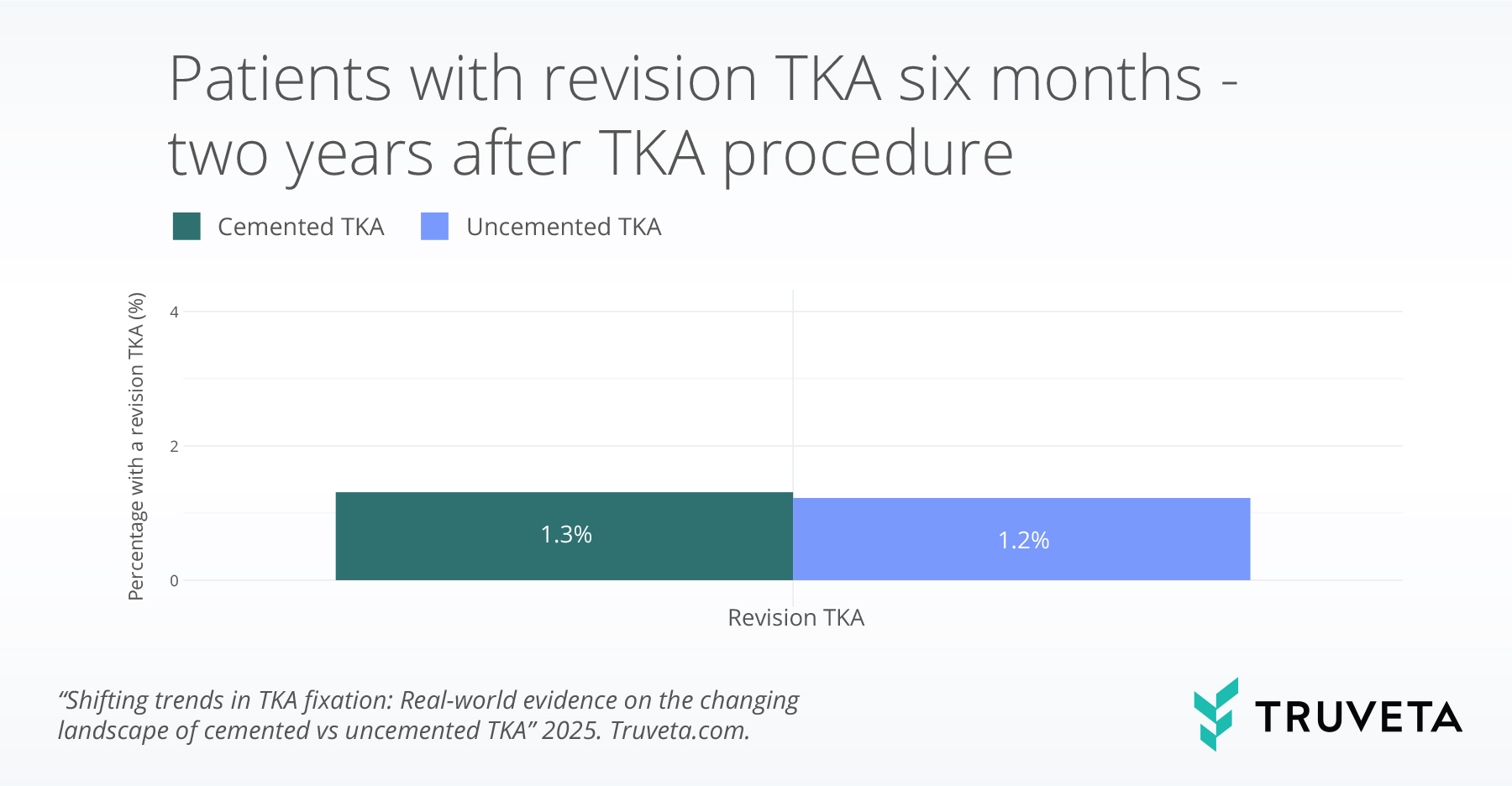
Revision by TKA type
We assessed revision TKA by fixation type. Rates of revision were low and comparable between cemented and uncemented TKAs (1.3% vs 1.2%). While older adults (75+) tended to have lower revision rates, the difference between cemented and uncemented TKAs did not vary significantly by age.
Discussion
In this study of inpatient total knee arthroplasty (TKA), we found that while cemented TKAs still represent the vast majority of fixations, the proportion of uncemented TKAs nearly doubled from 2018 to 2024. This upward trend has also been noted in prior literature, including analyses of national registries and claims databases, which have also reported increased adoption of uncemented techniques in recent years (20, 21).
Despite differences in patient demographics and clinical characteristics, uncemented and cemented TKAs had comparable short- and long-term outcomes. 30- and 90-day readmission rates were similar across fixation types, even when stratified by age. Likewise, rates of revision surgery within two years were low overall and did not significantly differ between cemented and uncemented TKAs. These findings suggest that uncemented TKAs do not pose an increased risk for hospital readmission or failure within two years of surgery.
However, our findings highlight notable differences in certain complications. While revision and readmission rates were similar, patients receiving cemented TKAs had consistently higher rates of early complications (e.g., instability, fractures, infections, and stiffness) and long-term complications (e.g., chronic pain). The literature comparing cemented and uncemented TKAs is mixed, with some studies reporting higher revision rates for uncemented implants, while others show comparable long-term outcomes and advantages in mechanical loosening and functional recovery (8, 9, 22–25).
Although some studies suggest that age has an impact on TKA outcomes, the literature is mixed, and findings often depend on the specific outcome being examined (26–29). In our age-stratified analyses, we found that while there were some age-related differences in early and long-term complications, readmission, and revision rates, the outcomes between cemented and uncemented TKAs were similar across all age groups. This suggests that uncemented fixation may perform as well as cemented fixation in both younger and older populations (8, 26), countering prior concerns about bone quality and implant stability in older adults. However, further research with longer follow-up is needed to confirm these results.
Several limitations should be considered when interpreting our findings. First, our analysis was limited to inpatient TKA procedures to be able to distinguish between cemented and non-cemented TKAs using ICD-10-PCS codes and does not include patients who underwent surgery in outpatient settings, which represent a growing proportion of TKAs in recent years. The number of inpatient TKAs has declined over time following CMS’s decision to remove TKA from the inpatient-only list (30). As a result, our findings may not be generalizable to those treated in outpatient or ambulatory surgical center settings. Future analyses could incorporate CPT and HCPCS codes to capture these outpatient procedures. Second, our follow-up period was limited to two years, which may not capture longer-term complications such as aseptic loosening, implant wear, or later revision surgery. Prior studies suggest that meaningful differences in implant longevity may emerge only over a 10- to 15-year horizon. Lastly, we did not include functional outcomes such as range of motion or patient-reported outcomes, limiting our ability to assess postoperative recovery and long-term physical function. Incorporating these outcomes in future studies will be important for a more comprehensive understanding of the relative performance of cemented and uncemented TKAs.
This study provides real-world evidence that uncemented TKAs not only have comparable outcomes to cemented TKAs, but in some cases are associated with lower rates of complications such as infection, instability, and chronic pain. These findings, derived from a large inpatient cohort, support the growing use of uncemented fixation as a viable alternative to cemented fixation. Further research, particularly with longer follow-up and inclusion of outpatient procedures, is needed to better understand the long-term performance and durability of uncemented implants.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on April 15, 2025. You can also view the complete report directly in Truveta Studio.
Citations
- D. Nam, C. M. Lawrie, R. Salih, C. R. Nahhas, R. L. Barrack, R. M. Nunley, Cemented Versus Cementless Total Knee Arthroplasty of the Same Modern Design: A Prospective, Randomized Trial. JBJS 101, 1185 (2019).
- P.-L. Xiao, C.-J. Hsu, Y.-G. Ma, D. Liu, R. Peng, X.-H. Xu, H.-D. Lu, Prevalence and treatment rate of osteoporosis in patients undergoing total knee and hip arthroplasty: a systematic review and meta-analysis. Arch Osteoporos 17, 16 (2022).
- F. Matassi, C. Carulli, R. Civinini, M. Innocenti, Cemented versus cementless fixation in total knee arthroplasty. Joints 01, 121–125 (2013).
- D. Dalury, Cementless total knee arthroplasty. The British Editorial Society of Bone & Joint Surgery 98, 867–873 (2016).
- T. Irmola, V. Ponkilainen, K. T. Mäkelä, O. Robertsson, A. W-Dahl, O. Furnes, A. M. Fenstad, A. B. Pedersen, H. M. Schrøder, A. Eskelinen, M. J. Niemeläinen, Association between fixation type and revision risk in total knee arthroplasty patients aged 65 years and older: a cohort study of 265,877 patients from the Nordic Arthroplasty Register Association 2000–2016. Acta Orthopaedica 92, 91–96 (2021).
- M. Daher, E. Mekhael, M. M. El-Othmani, Osteoporosis in the setting of knee arthroplasty: a narrative review. Arthroplasty 6, 50 (2024).
- K. Wang, H. Sun, K. Zhang, S. Li, G. Wu, J. Zhou, X. Sun, Better outcomes are associated with cementless fixation in primary total knee arthroplasty in young patients: a systematic review and meta-analysis of randomized controlled trials. Medicine 99, e18750 (2020).
- H. R. Mohammad, A. Judge, D. W. Murray, A Matched Comparison of the Long-Term Outcomes of Cemented and Cementless Total Knee Replacements: An Analysis from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man. JBJS 103, 2270 (2021).
- R. Monarrez, J. Dubin, S. S. Bains, D. Hameed, M. C. Moore, Z. Chen, M. A. Mont, R. E. Delanois, J. Nace, Cemented is not superior to cementless total knee arthroplasty for complications: a propensity score matched analysis. Eur J Orthop Surg Traumatol 34, 1825–1830 (2024).
- C. Chen, R. Li, Cementless versus cemented total knee arthroplasty in young patients: a meta-analysis of randomized controlled trials. J Orthop Surg Res 14, 262 (2019).
- K. B. Fricka, S. Sritulanondha, C. J. McAsey, To Cement or Not? Two-Year Results of a Prospective, Randomized Study Comparing Cemented Vs. Cementless Total Knee Arthroplasty (TKA). The Journal of Arthroplasty 30, 55–58 (2015).
- Y.-H. Kim, J.-W. Park, H.-M. Lim, E.-S. Park, Cementless and cemented total knee arthroplasty in patients younger than fifty five years. Which is better? Int Orthop 38, 297–303 (2014).
- B. Feng, J. Lin, J. Jin, W.-W. Qian, W. Wang, X.-S. Weng, Thirty-day Postoperative Complications following Primary Total Knee Arthroplasty: A Retrospective Study of Incidence and Risk Factors at a Single Center in China. Chin Med J (Engl) 130, 2551–2556 (2017).
- A. J. Metoxen, A. C. Ferreira, T. S. Zhang, M. A. Harrington, M. J. Halawi, Hospital Readmissions After Total Joint Arthroplasty: An Updated Analysis and Implications for Value-Based Care. The Journal of Arthroplasty 38, 431–436 (2023).
- J. Benito, J. Stafford, H. Judd, M. Ng, A. Corces, M. W. Roche, Length of Stay Increases 90-day Readmission Rates in Patients Undergoing Primary Total Joint Arthroplasty. J Am Acad Orthop Surg Glob Res Rev 6, e21.00271 (2022).
- H. Chawla, J. P. Van Der List, A. B. Christ, M. R. Sobrero, H. A. Zuiderbaan, A. D. Pearle, Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis. The Knee 24, 179–190 (2017).
- R. A. Sershon, N. Tecle, C. J. Della Valle, B. R. Levine, R. A. Berger, D. Nam, The Impact of an Acute, Traumatic Wound Dehiscence on Clinical Outcomes Following Primary Knee Arthroplasty. J Arthroplasty 33, 2613–2615 (2018).
- M. R. Bong, P. E. Di Cesare, Stiffness after total knee arthroplasty. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 12, 164–171 (2004).
- S. P. Ryan, J. B. Stambough, J. I. Huddleston, B. R. Levine, Highlights of the 2023 American Joint Replacement Registry Annual Report. Arthroplasty Today 26, 101325 (2024).
- A. R. Agarwal, E.-V. Kuyl, A. Gu, G. J. Golladay, S. C. Thakkar, G. Siram, A. Unger, S. Rao, Trend of using cementless total knee arthroplasty: a nationwide analysis from 2015 to 2021. Arthroplasty 6, 24 (2024).
- “American Joint Replacement Registry (AJRR): 2024 Annual Report” (American Academy of Orthopaedic Surgeons (AAOS), 2024).
- C. U. Gwam, N. E. George, J. I. Etcheson, S. Rosas, J. F. Plate, R. E. Delanois, Cementless versus Cemented Fixation in Total Knee Arthroplasty: Usage, Costs, and Complications during the Inpatient Period. J Knee Surg 32, 1081–1087 (2019).
- H. Yazdi, K. J. Choo, C. Restrepo, M. Hammad, M. Sherman, J. Parvizi, Short-term results of triathlon cementless versus cemented primary total knee arthroplasty. The Knee 27, 1248–1255 (2020).
- D. Chiou, A. K. Li, A. Upfill-Brown, A. Arshi, P. Hsiue, K. Chen, A. Stavrakis, C. D. Photopoulos, Cementless compared to cemented total knee arthroplasty is associated with more revisions within 1 year of index surgery. Arthroplasty Today 21, 101122 (2023).
- M. Mercurio, G. Gasparini, V. Sanzo, F. Familiari, D. Castioni, O. Galasso, Cemented Total Knee Arthroplasty Shows Less Blood Loss but a Higher Rate of Aseptic Loosening Compared With Cementless Fixation: An Updated Meta-Analysis of Comparative Studies. The Journal of Arthroplasty 37, 1879-1887.e4 (2022).
- A. R. Maniar, J. L. Howard, L. E. Somerville, B. A. Lanting, E. M. Vasarhelyi, Cementless Total Knee Arthroplasty: Does Age Affect Survivorship and Outcomes? The Journal of Arthroplasty 39, S95–S99 (2024).
- L. Townsend, R. Roubion, D. Bourgeois, C. Leonardi, R. Fox, V. Dasa, G. Pollock, Impact of Age on Patient-Reported Outcome Measures in Total Knee Arthroplasty. J Knee Surg 31, 580–584 (2018).
- M. Fang, N. Noiseux, E. Linson, P. Cram, The Effect of Advancing Age on Total Joint Replacement Outcomes. Geriatr Orthop Surg Rehabil 6, 173–179 (2015).
- J. Julin, E. Jämsen, T. Puolakka, Y. T. Konttinen, T. Moilanen, Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis: A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthopaedica 81, 413–419 (2010).
- US Department of Health and Human Services, Total Knee Arthroplasty (TKA) Removal from the Medicare Inpatient-Only (IPO) List and Application of the 2-Midnight Rule | Guidance Portal (2019). https://www.hhs.gov/guidance/document/total-knee-arthroplasty-tka-removal-medicare-inpatient-only-ipo-list-and-application-2.

