Authors: Amy Austin, MS ⊕Truveta, Inc, Bellevue, WA, Emily Webber, PhD ⊕Truveta, Inc, Bellevue, WA, Sarah Blach, MS ⊕Truveta, Inc, Bellevue, WA, Jared Kern ⊕Truveta, Inc, Bellevue, WA, Sarah Platt, MS ⊕Truveta, Inc, Bellevue, WA, Sally Omidvar, MSPH, MS ⊕Truveta, Inc, Bellevue, WA, Michael Mack, MD ⊕Baylor Scott & White Health, Dallas, TX, Michael R. Jaff, DO ⊕Boston Scientific, Marlborough, MA
- Adding a “highest risk” category to pulmonary embolism (PE) risk stratification reveals substantial differences in mortality, treatment use, and length of stay.
- Truveta’s expanded approach enables more granular identification of patients most in need of advanced interventions.
This blog is an extension of our poster presented at the International Society for Pharmacoepidemiology Annual Meeting (ISPE), titled A real-world risk stratification approach to pulmonary embolism using Truveta Data.
Pulmonary embolism is a life-threatening condition with a one-year mortality rate of approximately 14% and a 30-day mortality rate of about 4%. Risk stratification is essential for guiding clinical decisions. The simplified Pulmonary Embolism Severity Index (sPESI) is widely used but has only two risk categories.
Objective: Evaluate whether adding a “highest risk” category can better differentiate outcomes among high-risk PE patients using real-world electronic health record (EHR) data.
Methods
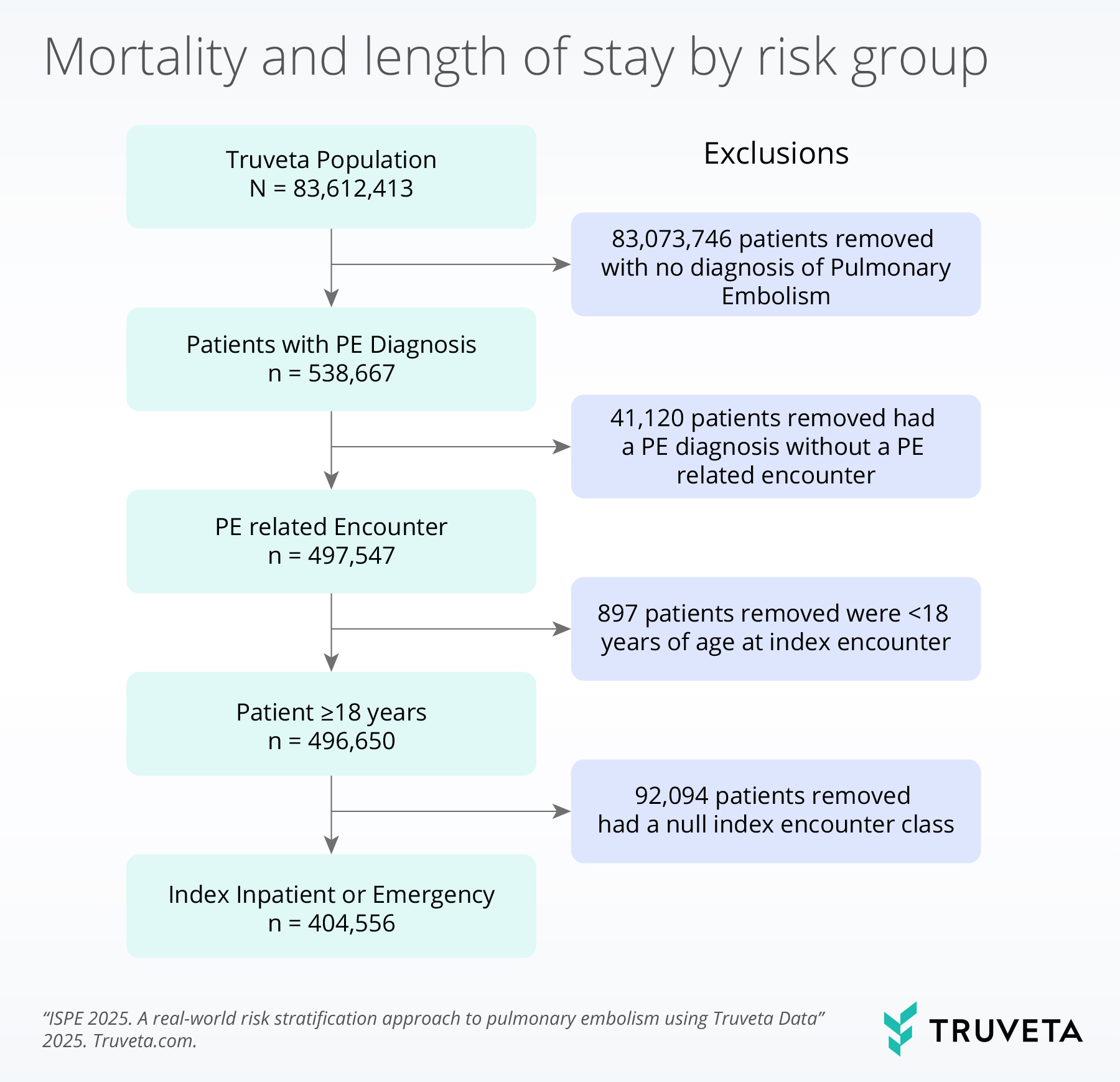
We conducted a retrospective analysis using Truveta Data, which provides daily updated, de-identified electronic health record (EHR) data from leading US health systems, including hospitals and clinics, representing over 120 million patients.
Using Truveta Data, we identified adults aged 18 years or older with an initial PE diagnosis (using ICD-10 or SNOMED codes) during inpatient or emergency encounters between January 1, 2016 and April 30, 2024.
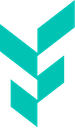
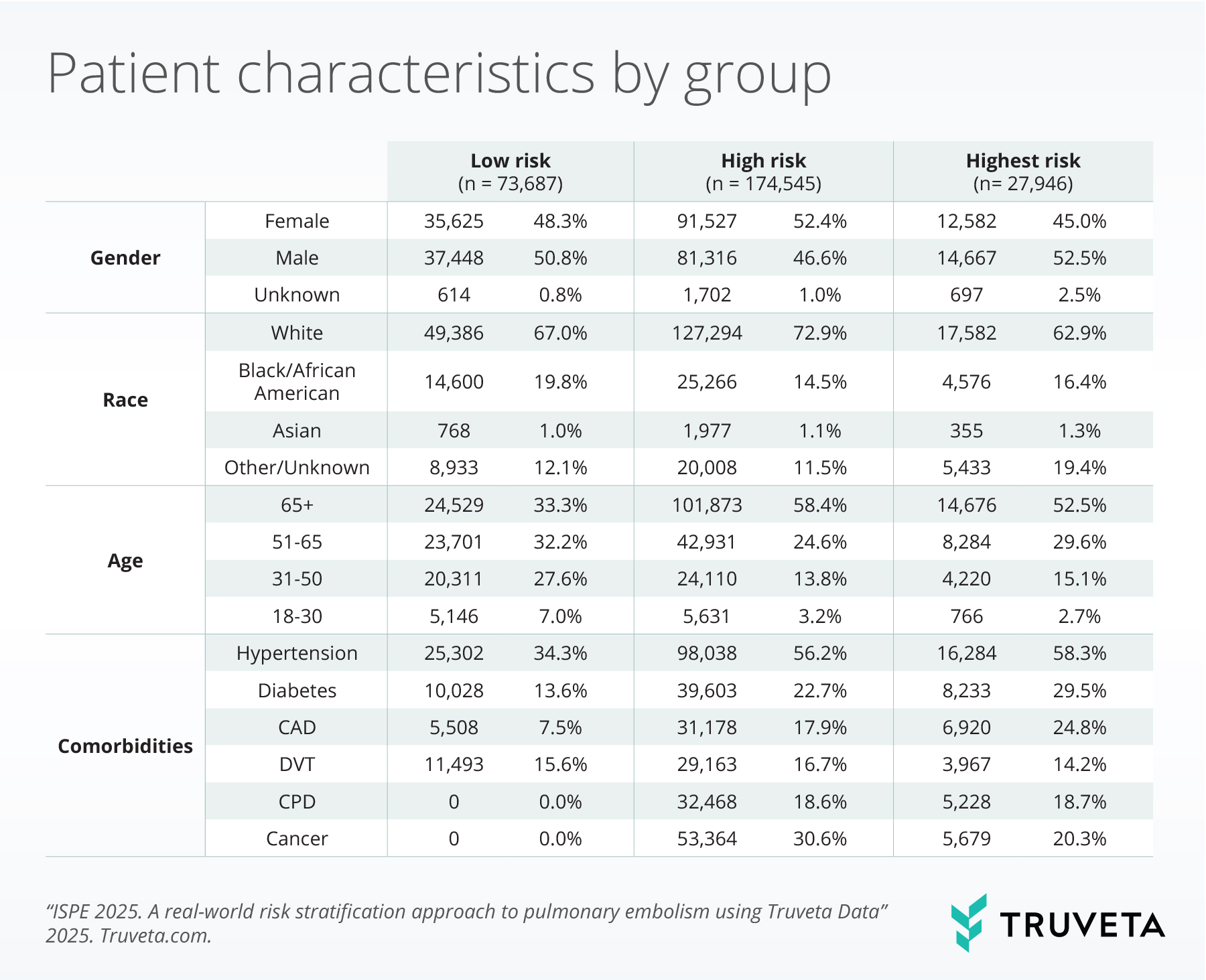
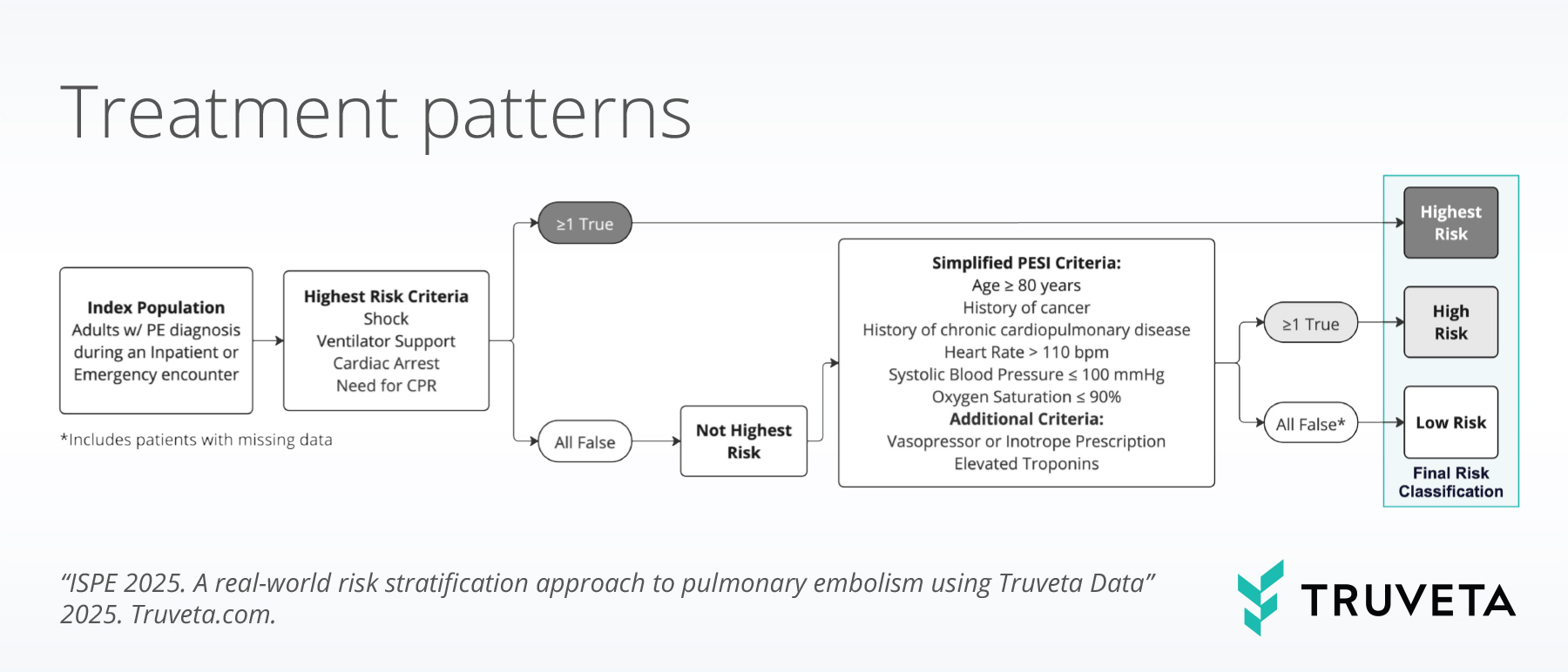
Patients were stratified into three risk categories:
• Highest risk: Shock, mechanical ventilation, cardiac arrest, or CPR within 1 day of diagnosis.
• High risk: sPESI > 0, elevated troponin, or vasopressor/inotrope use within 1 day of diagnosis.
• Low risk: Did not meet any of the criteria above.
Treatment categories were classified as:
• Advanced therapy (AT): Surgical thrombectomy, catheter-directed thrombolysis, catheter-based mechanical thrombectomy, systemic tPA.
• Medication-only therapy (MOT): Anticoagulants (LMWH, UFH, DOACs, warfarin).
Analyses included descriptive statistics, chi-square tests, and outcome comparisons.
Results
The analysis resulted in a population of 276,178 patients with first-time PE. Among these patients, the mean age was 63.3 years, with 50.6% female and 73.3% White.
Risk distribution
In evaluating the risk distribution, 62.2% of patients were identified as high risk, 26.7% as low risk, and 10.1% as highest risk.
Treatment patterns
Advanced therapy (AT) was used for 17.8% of patients with highest risk, 8.8% of patients with high risk, and 3.0% of patients with low risk.
Medication-only treatment (MOT) was used for 67.8% of patients with highest risk, 81.4% of patients with high risk, and 71.5% of patients with low risk.
Outcomes
The 30-day inpatient mortality was 29.9% for patients with highest risk, 5.2% for patients with high risk, and 1.3% among patients with low risk.
The mean length of stay in the hospital was greatest among patients with highest risk (11.9 days), the decrease for patients with high risk (7.0 days) and low risk (5.7 days).
Discussion
Adding a “highest risk” category improves stratification, identifying patients with significantly higher mortality and longer hospital stays who may benefit from advanced interventions.
These findings are consistent with data accessed on May 6, 2024.