Authors: Mantas Dmukauskas, PhD ⊕Truveta, Inc, Bellevue, WA, Sarah Blach, MS ⊕Truveta, Inc, Bellevue, WA, Sunny Guin, PhD ⊕Truveta, Inc, Bellevue, WA, Amy Wu ⊕Truveta, Inc, Bellevue, WA
- The survival rate for patients with glioblastoma (GBM) differs significantly by age, sex, race, and comorbidity burden.
- Truveta’s large real-world dataset enables more robust survival analysis than prior studies, with adjustments for comorbidities.
This blog is an extension of our poster presented at the International Society for Pharmacoepidemiology Annual Meeting (ISPE), titled Real-world data survival patterns in glioblastoma patients.
Glioblastoma multiforme (GBM) is the most common malignant brain tumor, representing 16% of all primary brain and central nervous system tumors in the US. Adults diagnosed with GBM face a poor prognosis, with median overall survival of around 15 months. Previous studies have identified demographic and clinical factors influencing GBM survival but often lacked adjustments for comorbidities or were limited by small sample sizes.
Our research question: How do survival outcomes vary by age, sex, race, and comorbidity burden in GBM patients when analyzed using Truveta’s large, real-world dataset?
The results show that demographics—particularly age and comorbidity score—are strong predictors of GBM survival in real-world clinical practice.
Methods
We conducted a retrospective analysis using Truveta Data, which provides daily updated, de-identified electronic health record (EHR) data from leading US health systems, including hospitals and clinics, representing over 120 million patients.
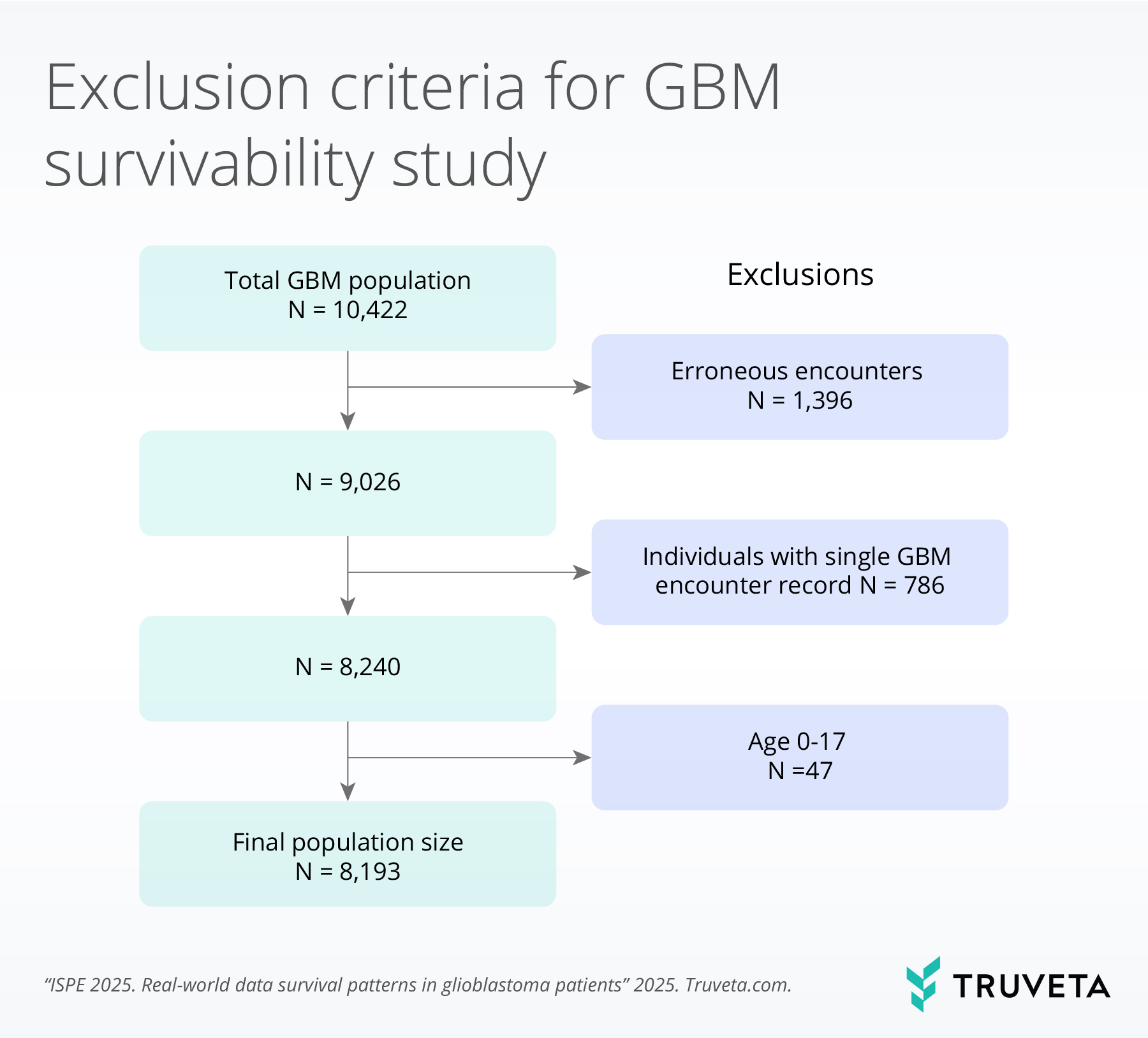
Using Truveta Data, we identified adults aged 18 and older with a confirmed GBM diagnosis and more than one GBM-related encounter.
Patients were excluded if there was low confidence in the diagnosis, they had only one encounter related to GBM, and if they were under the age of 18.
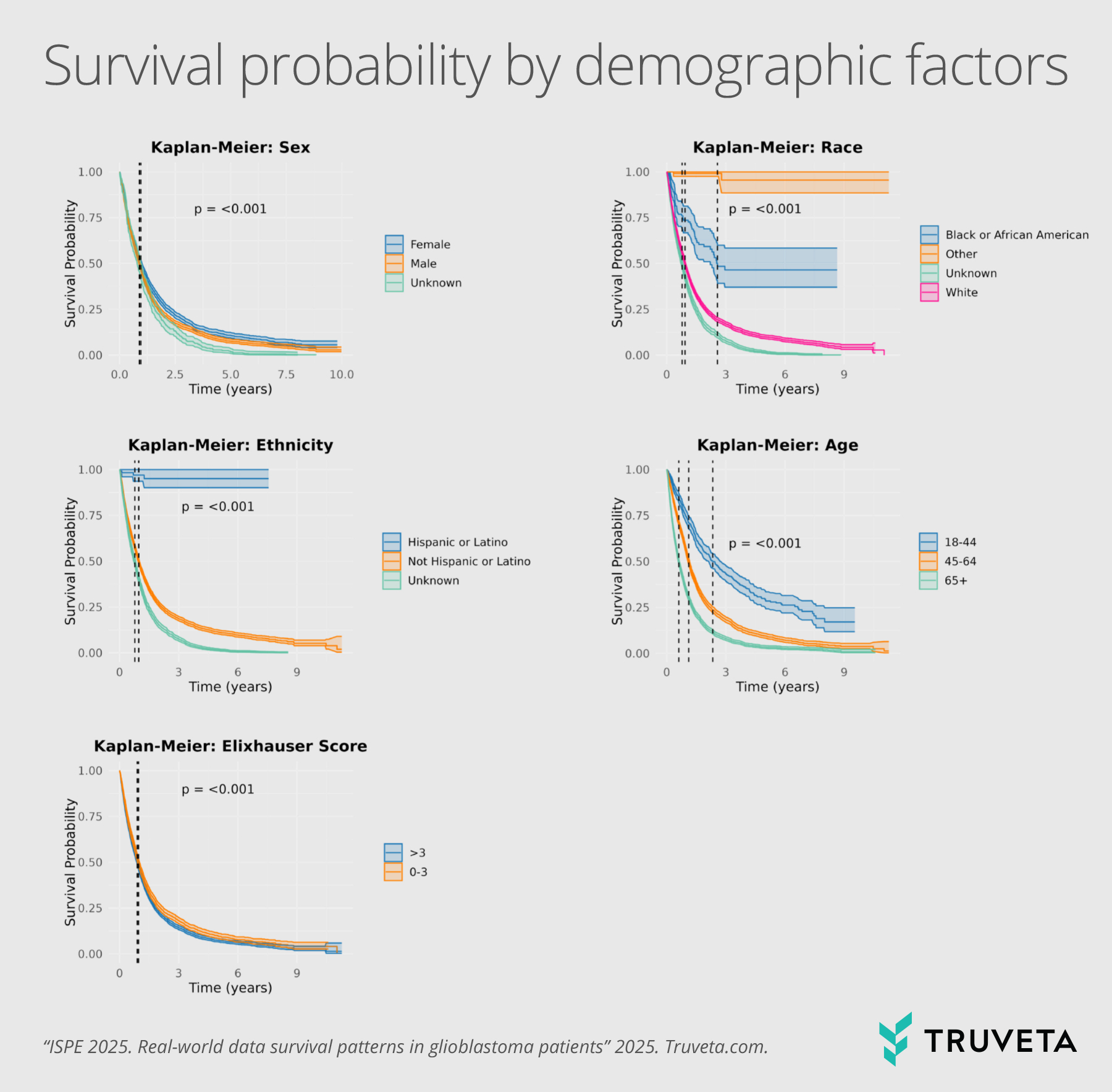
We used Kaplan-Meier survival curves and Cox proportional hazards models to conduct the analysis, adjusting for Elixhauser comorbidity score, age, sex, and race.
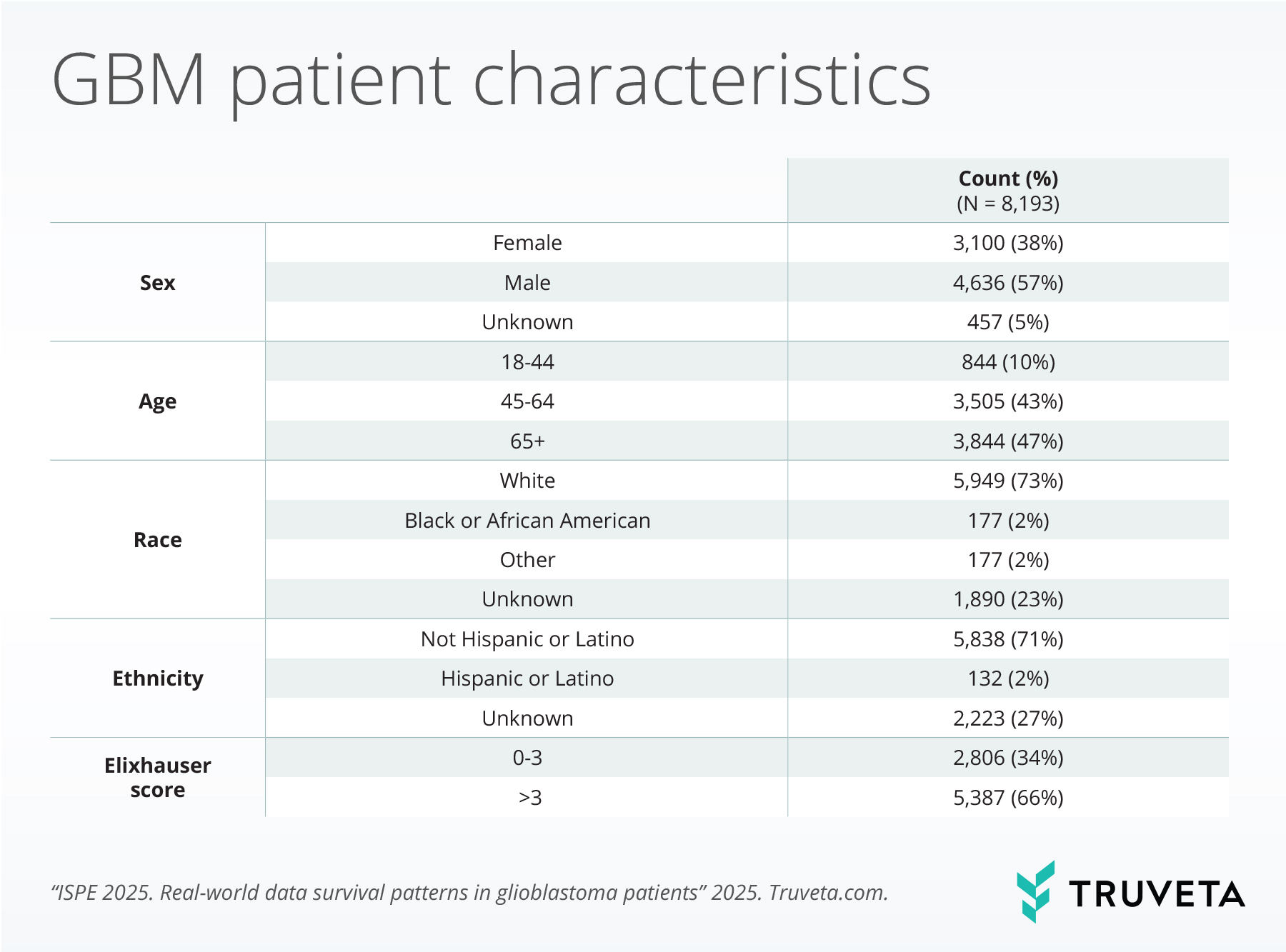
We identified 8,193 patients for final analysis who met study criteria.
Results
Survival by demographic factors, such as age, sex, and race, differed among patients with GBM:
- Age: Older patients had significantly shorter survival times.
- In the Kaplan Meyer survival curves, survivability for patients aged 65 years and older was 7.3 months, compared to patients aged 18-44 (28 months) and patients aged 45-64 (13.4 months, p<0.001).
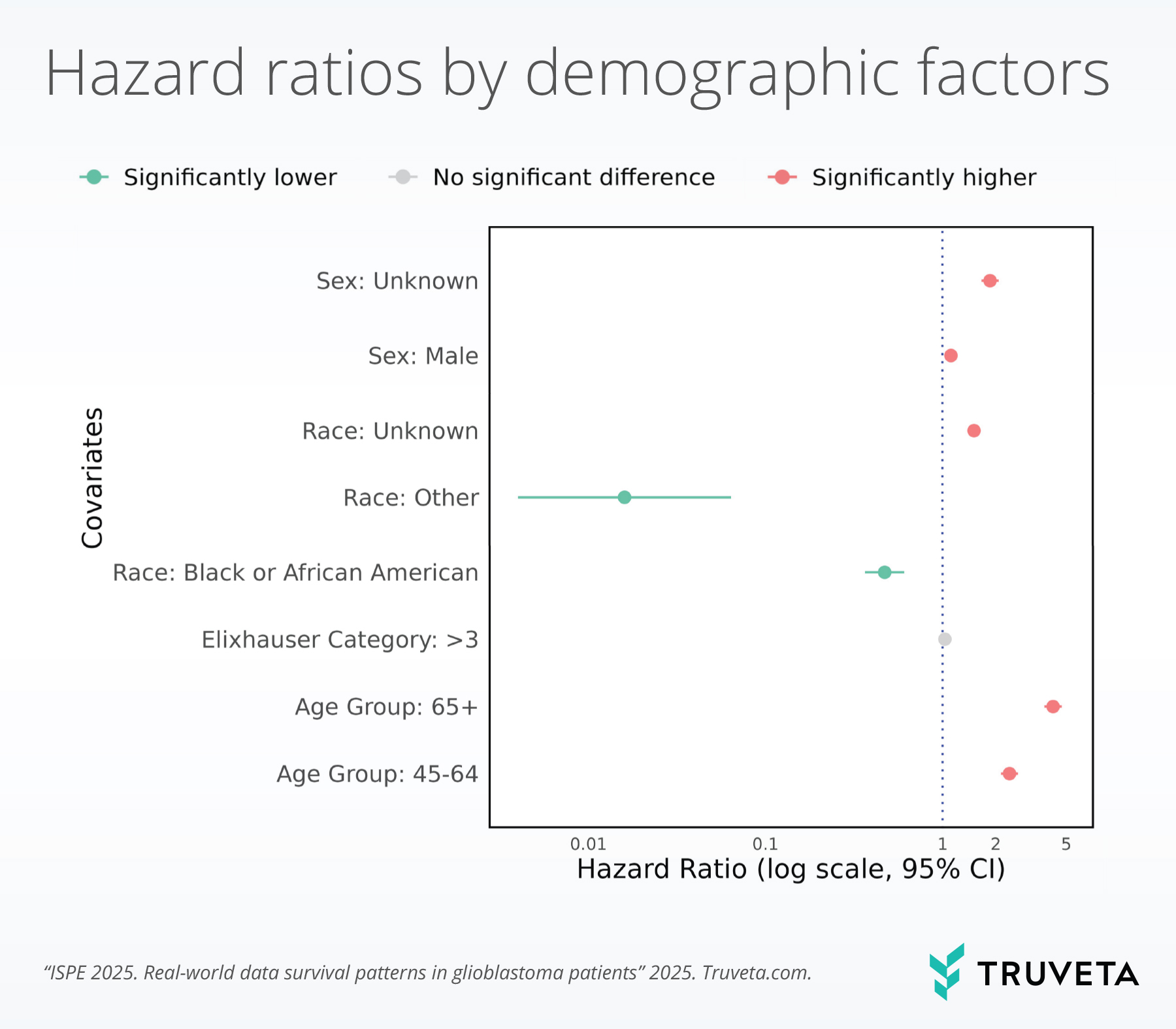
- When adjusting for covariates using the Cox proportional hazard model, patients aged 45-64 had a hazard ratio (HR) of 2.39 (95% CI: 2.14-2.66, p<0.001), and patients aged 65 or older had a hazard ratio (HR) of 4.21 (95% CI: 3.76-4.71, p<0.001).
- Sex: Male patients had shorter survival compared to female patients.
- In the Kaplan Meyer survival curves, survivability for male patients was 10.8 months compared to female patients at 11.5 months (p<0.001).
- When adjusting for covariates using the Cox proportional hazard model, significantly higher hazard ratios (HR) were observed in males (HR = 1.12, 95% CI: 1.06-1.18, p<0.001) compared to females.
- Race: Racial differences in survival were observed, though less pronounced than age effects. White patients had a median survival of 11.1 months, compared to 30.8 months for Black patients.
Higher Elixhauser comorbidity scores were associated with worse survival outcomes, independent of age and other factors. Patients with a higher baseline Elixhauser score had shorter survival (score of ≥3 vs. 0-3; 10.7 vs. 11.5 months).
Discussion
Our findings confirm that patient demographics and comorbidity burden are strong predictors of GBM survival, consistent with prior literature, but now demonstrated in a large, real-world dataset that allows for more nuanced adjustment and subgroup analysis. These results underscore the importance of considering both demographic and comorbidity factors in GBM prognosis and care planning.
These findings are consistent with data accessed in December 2024.
Citations
- Nizamutdinov, D. et al. Prognostication of Survival Outcomes in Patients Diagnosed with Glioblastoma. World Neurosurgery 109, e67–e74 (2018).
- Carr MT, Hochheimer CJ, Rock AK, Dincer A, Ravindra L, Zhang FL, Opalak CF, Poulos N, Sima AP, Broaddus WC. Comorbid Medical Conditions as Predictors of Overall Survival in Glioblastoma Patients. Sci Rep. 2019 Dec 27;9(1):20018. doi:10.1038/s41598-019-56574-w.