Gestational diabetes is one of the most common complications of pregnancy, affecting roughly 5–9% of pregnancies in the United States. When diagnosed and managed early, patients can avoid complications such as high birth weight, preterm delivery, or cesarean section. However, gestational diabetes can also be associated with long-term risks for both parent and baby, including type 2 diabetes, cardiovascular disease, and obesity.
In this Truveta experts spotlight, Brianna Cartwright, MS, shares new insights on how gestational diabetes screening is performed in real world . Brianna is a Principal Research Analyst who leads the insights team on Truveta Research. Her recent work has focused on public health, with expertise spanning vaccine administration, mental health, GLP-1 therapies, and pandemic impacts.
Her latest analysis explores Truveta Data to reveal how screening values are distributed, how results vary by maternal age, and whether patients are being tested within the recommended gestational window.
Why it matters
Guidelines recommend that all pregnant women be screened for gestational diabetes between 24 and 28 weeks of pregnancy. Screening is typically done with a 1-hour glucose challenge test, where results above indicate the need for further testing (and results above 130mg/dL can prompt a re-take). Real-world evidence on how consistently these recommendations are followed—and which patients are more likely to have abnormal results—can inform public health interventions and help close gaps in prenatal care.
“Examining real-world lab values is an especially powerful aspect of real-world data. By looking at lab test results alongside gestational age and demographics, researchers can see whether women are screened at the right time and which populations face higher risk for additional complications.” – Brianna Cartwright, MS
Methods
Using Truveta Data, Brianna identified 505,475 women ages 16–50 who underwent gestational diabetes screening between 2018 and July 2025. Screening values were captured using the standard LOINC code for the 1-hour glucose challenge test.
- Screening classification: Screening results were categorized as follows: values >140 mg/dL were considered a failed screen, values 130–140 mg/dL as a stricter fail threshold used in some practices, and values <130 mg/dL as a passed screen.
- Age comparisons: We summarized the distribution of test values and the proportion screen-positive across maternal age groups.
- Timing of screening: When gestational-age codes were available, we flagged whether the test occurred within the recommended 24–28-week window.
Results
76.4% of screening values fell below the 140 mg/dL threshold, while the remainder flagged potential risk warranting follow-up testing.
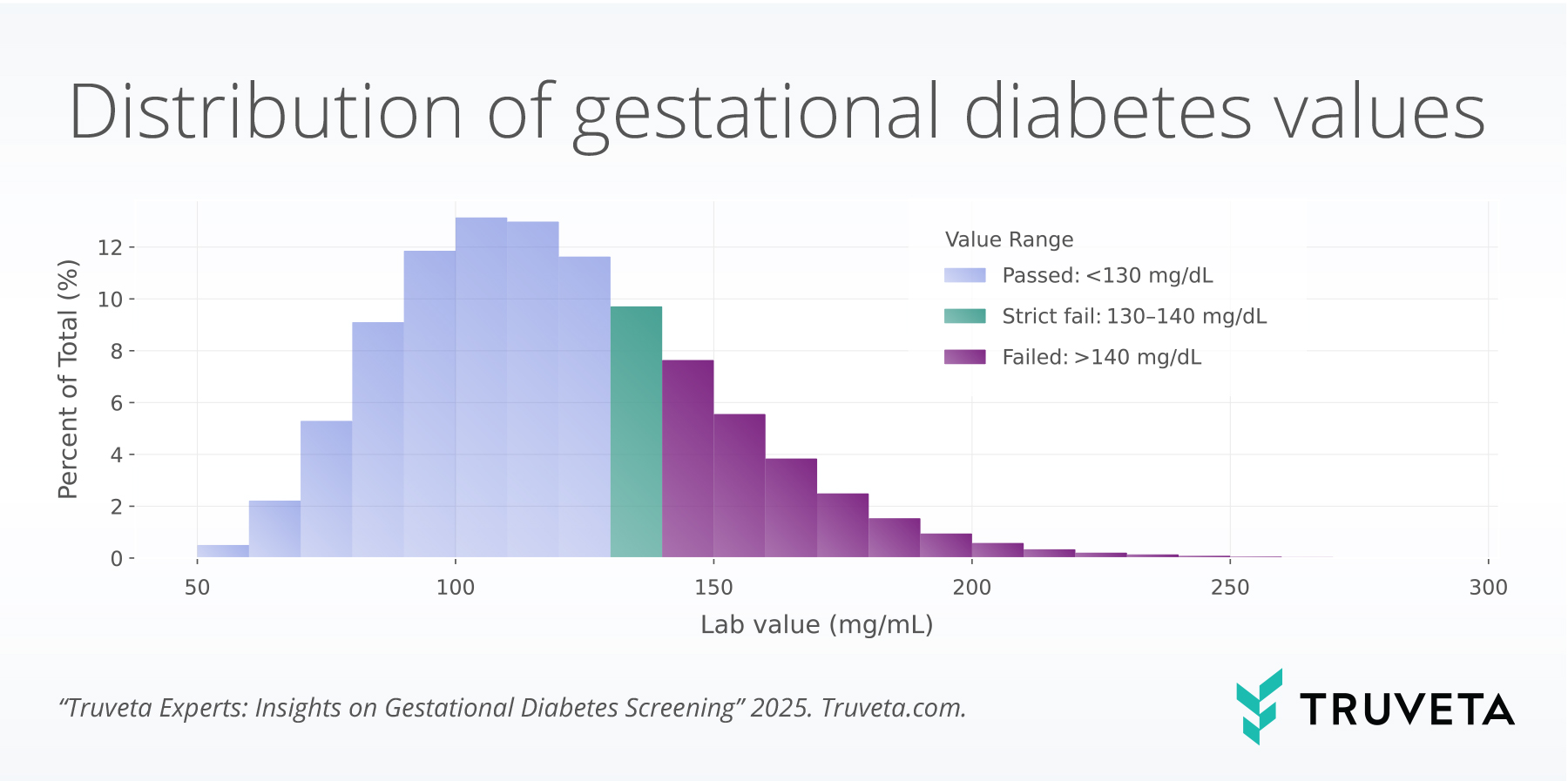
Figure 1. Distribution of gestational diabetes screening values, stratified by maternal age.
Average screening values increased with maternal age, consistent with known risk patterns.
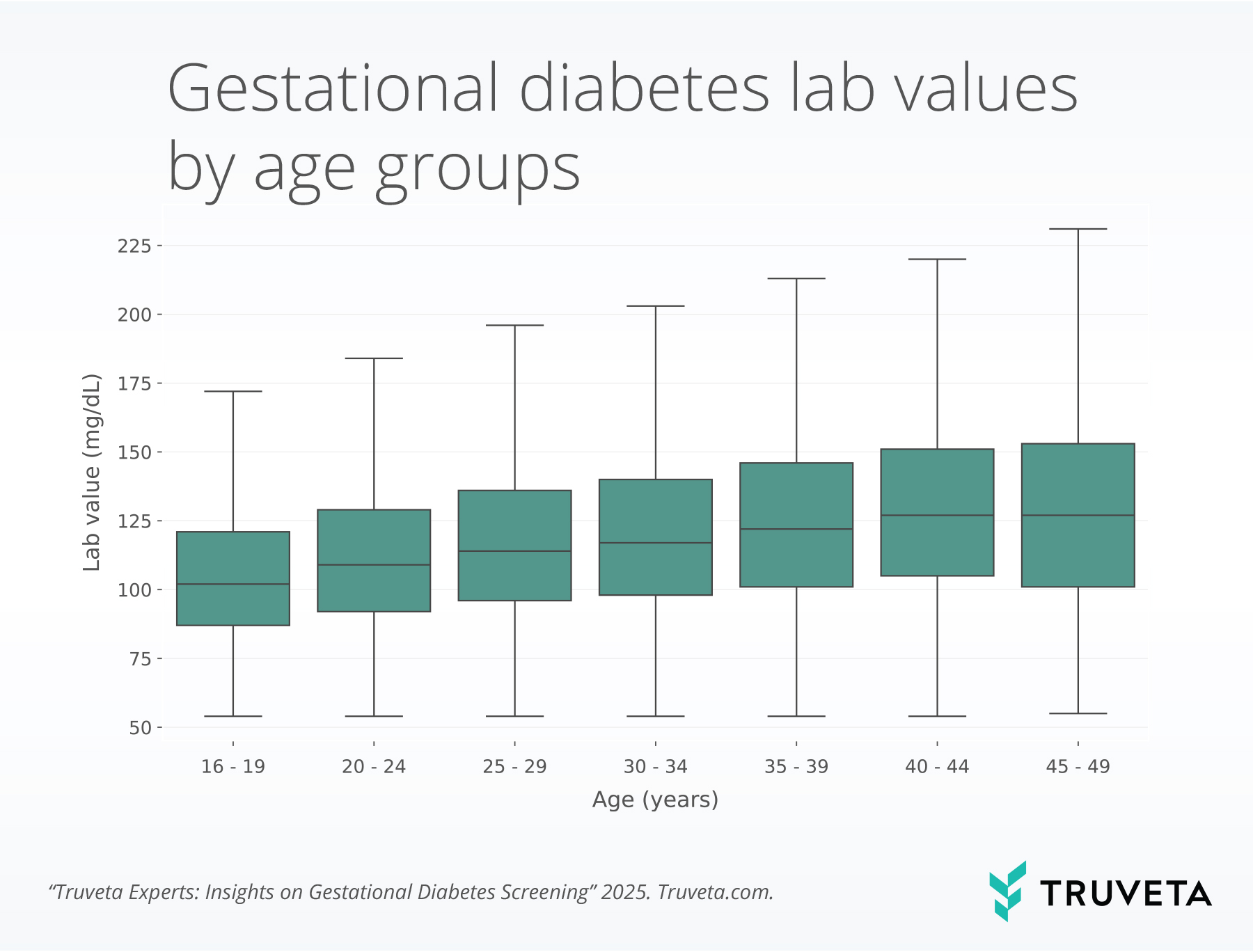
Figure 2. Gestational diabetes lab values by age group, 2018–2025.
67.1% of patients were screened within the recommended 24–28-week window; the rest were tested earlier or later, suggesting variation in care timing.

Figure 3. Timing of screening relative to gestational age, 2018–2025.
How Truveta Data enabled this insight
- Standardized lab values (provided consistent screening measures across health systems)
- Integrated demographics and labs created a unified view to assess screening value distributions and age correlations in real-world clinical practice
Discussion
This analysis reveals that while most patients undergo gestational diabetes screening within the recommended gestational age range, nearly one-third are tested earlier or later, which could impact diagnostic accuracy. Providers may order earlier tests for women with elevated baseline risk factors such as prior gestational diabetes, obesity, prediabetes, or advanced maternal age, or in response to clinical signs like glycosuria or elevated random glucose. Conversely, delays may stem from missed visits, late entry to prenatal care, or scheduling barriers.
Higher screening values in older age groups align with known risk factors for gestational diabetes and may justify closer monitoring in these populations. Supporting this, CDC data indicates that gestational diabetes diagnoses rose from 6.0% in 2016 to 8.3% in 2021, with prevalence increasing steadily with age—15.6% in mothers aged ≥40 versus 2.7% in those <20.
While most pregnant women are being evaluated for gestational diabetes according to clinical criteria, there is a significant group of pregnant women who may not be getting treatment that follows best-practice guidelines. By capturing not only screening results but also the timing and context of testing, Truveta Data offers a real-world lens into when and why deviations occur, helping identify opportunities to improve maternal and fetal outcomes.
About Truveta experts
The Truveta experts series highlights insights from researchers, clinicians, and data scientists working across Truveta. Each post highlights how real-world data can unlock new understanding—from disease patterns to treatment complexity to population health trends.
Explore more in this series:
Treatment trends for trigeminal neuralgia
Fireworks during the fourth of July
Real-world trends in Rituxan biosimilar adoption
Sudden cardiac arrest and arrhythmias among patients with chronic kidney disease
Biomarker testing trends in metastatic non-small cell lung cancer
Request a customized demo to see how Truveta Data can accelerate your next study.
