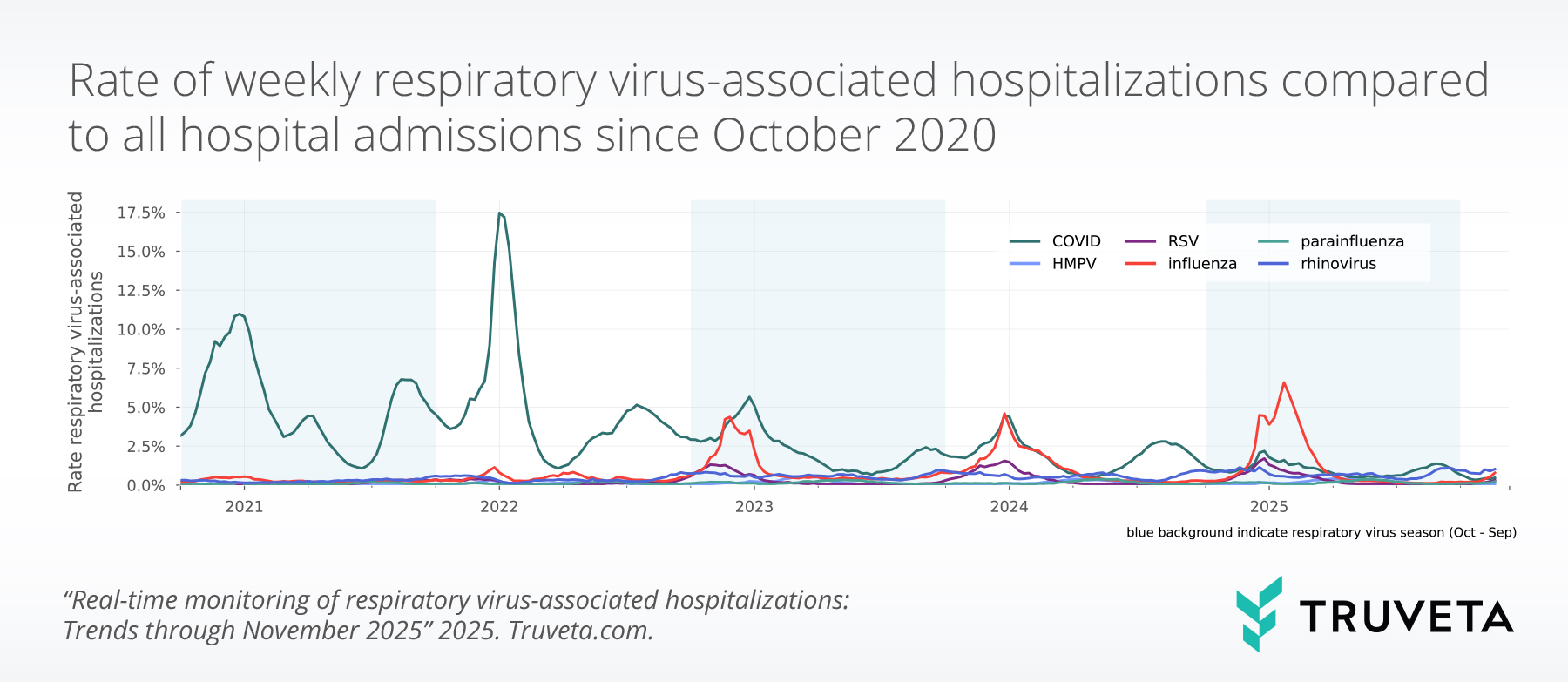
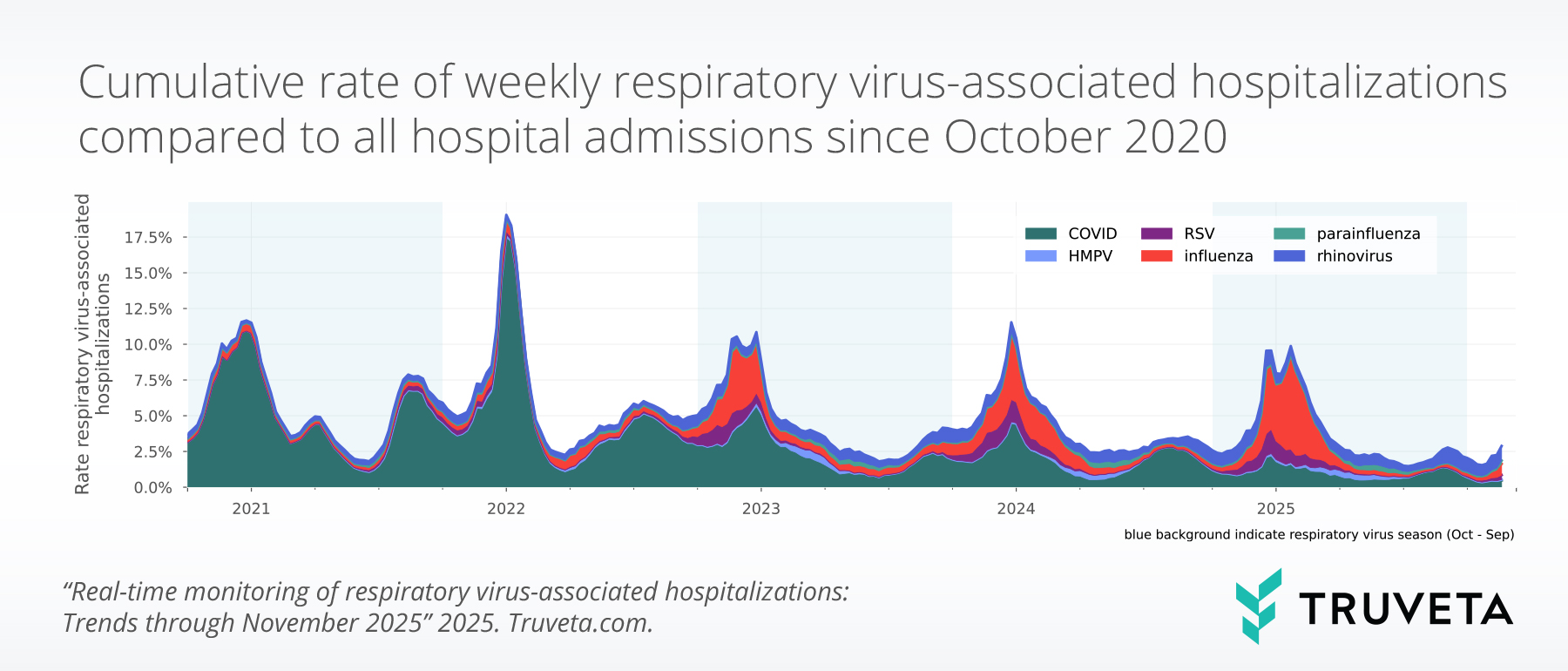
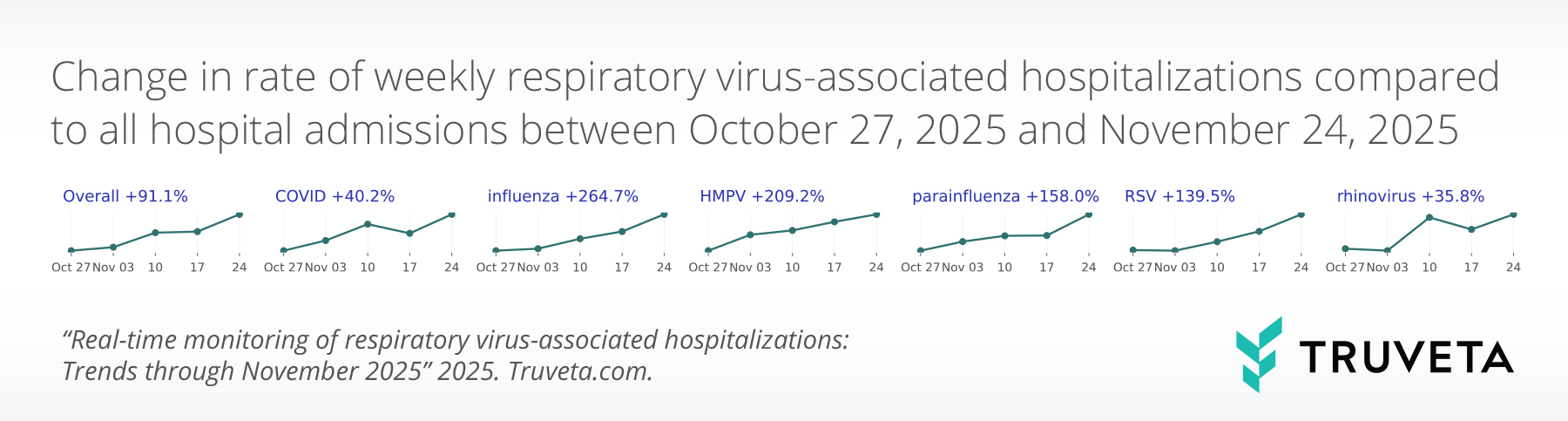
- Respiratory virus–associated hospitalizations increased overall in November 2025 (+91.1%) and now make up 2.5% of all hospitalizations.
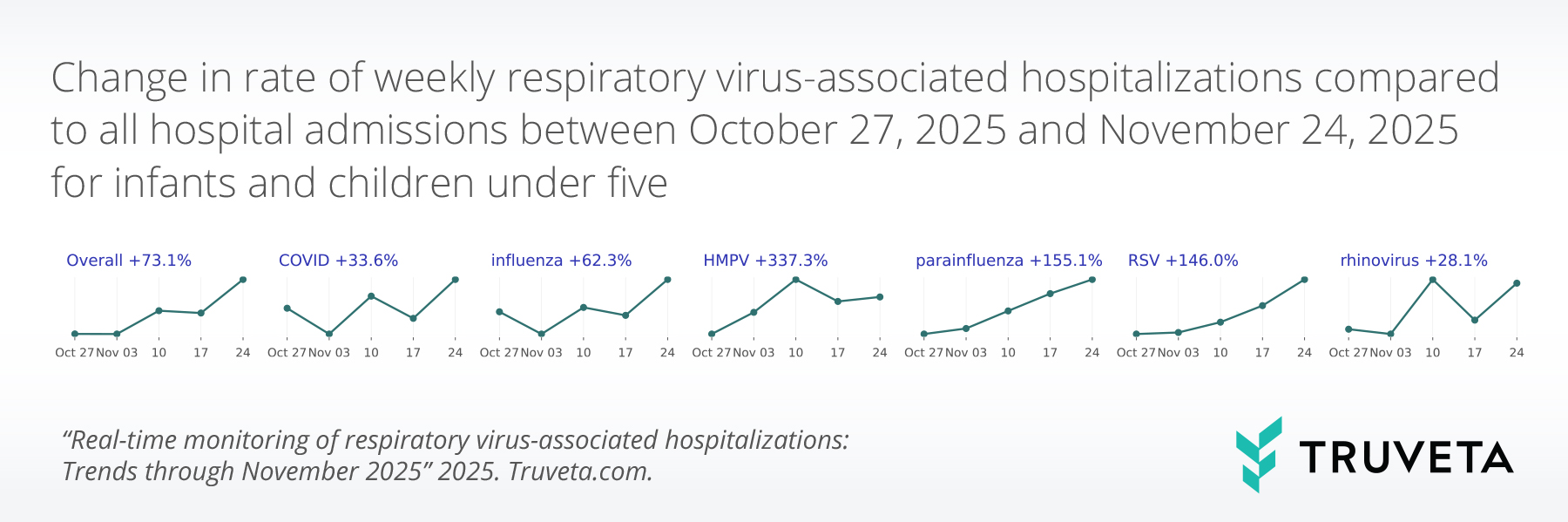
- Respiratory virus–associated hospitalizations increased substantially among children aged 0-4 years old (+73.1%), reaching 3.9% of all hospitalizations.
- RSV-associated hospitalizations in children aged 0-4 years old more than doubled for the third consecutive month and now account for 1.5% of hospitalizations in this age group.
Because Truveta Data provides the most complete, timely, and clean de-identified EHR data, including full patient medical records, notes, and images, linked with closed claims for more than 120 million patients across the US, we can show the latest trends in these respiratory virus-associated hospitalizations, including valuable insight into two at-risk populations: infants and children (age 0-4 years old) and older adults (age 65 and over).
This report provides a snapshot of the key findings with data through November 30, 2025 in the report specific to the overall population across all respiratory viruses, as well as for two high-risk populations: infants and children (age 0-4 years old) and older adults (age 65 and older). For the full analysis—inclusive of demographics, comorbidities, and overall trends in virus-associated hospitalizations and testing across all age groups for each virus—see the complete report with data through November 30, 2025 on MedRxiv.
Key findings: Trends in respiratory virus-associated hospitalizations
Overall hospitalization rates increasing
Pediatric respiratory virus-associated hospitalizations increasing substantially
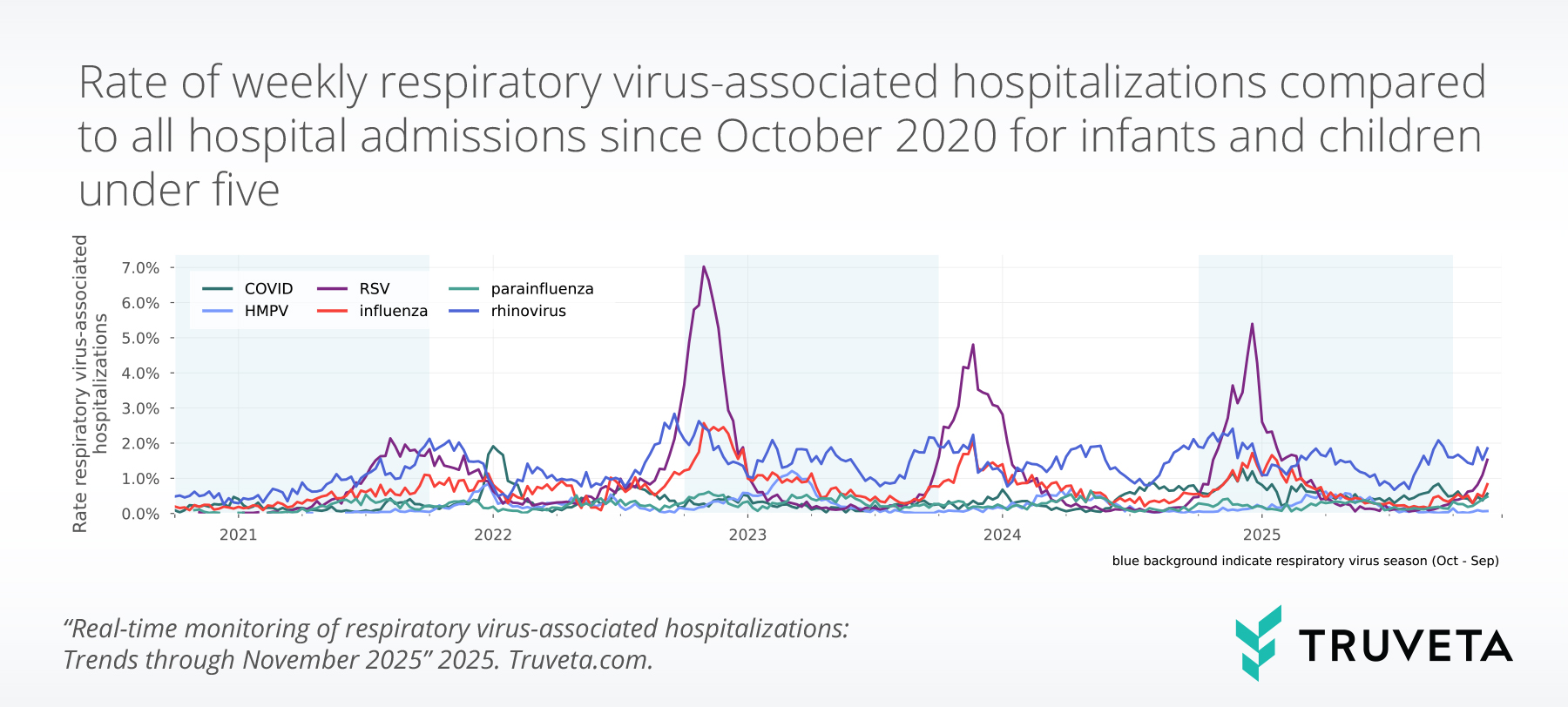
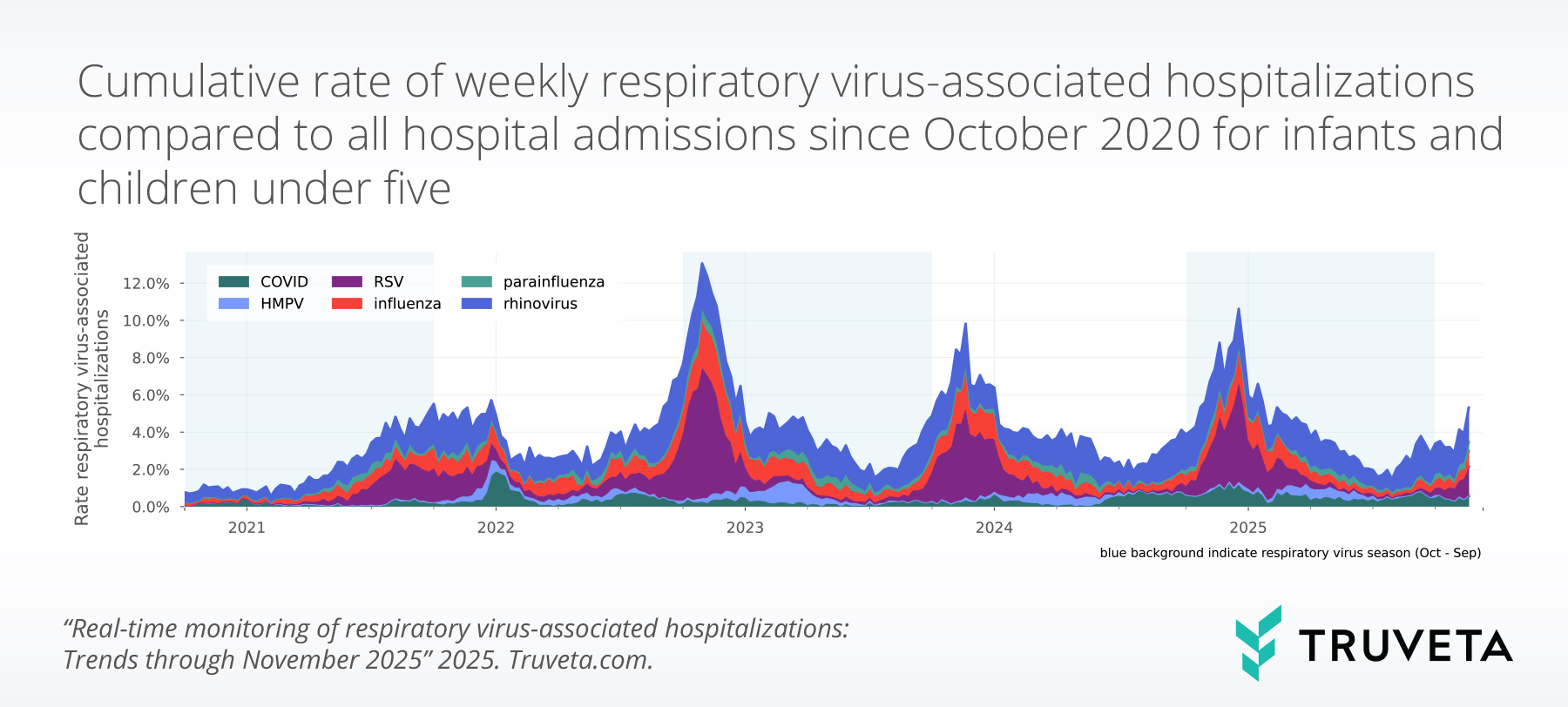
Influenza- and parainfluenza- associated hospitalizations also increased, while COVID- and rhinovirus- associated hospitalizations increased more modestly.
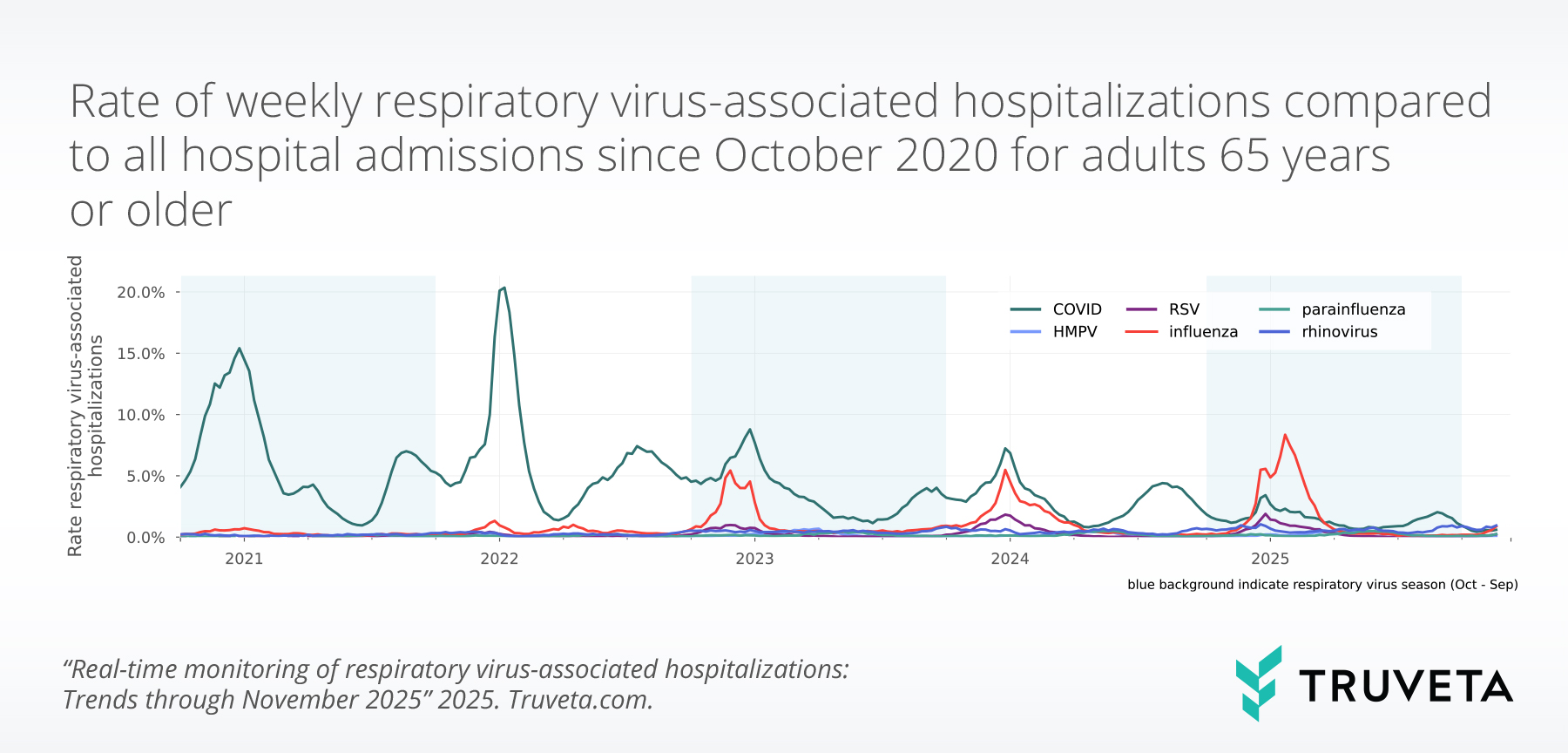
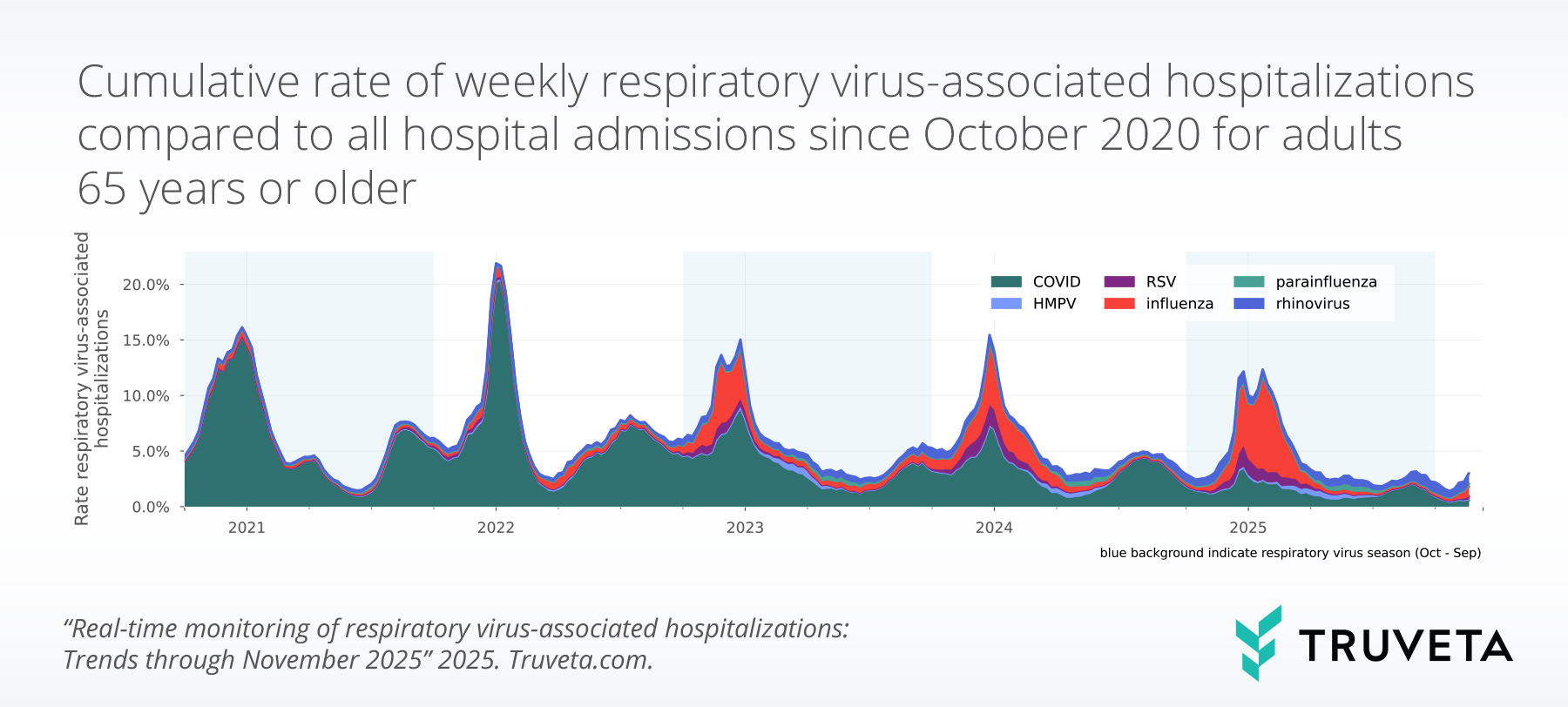
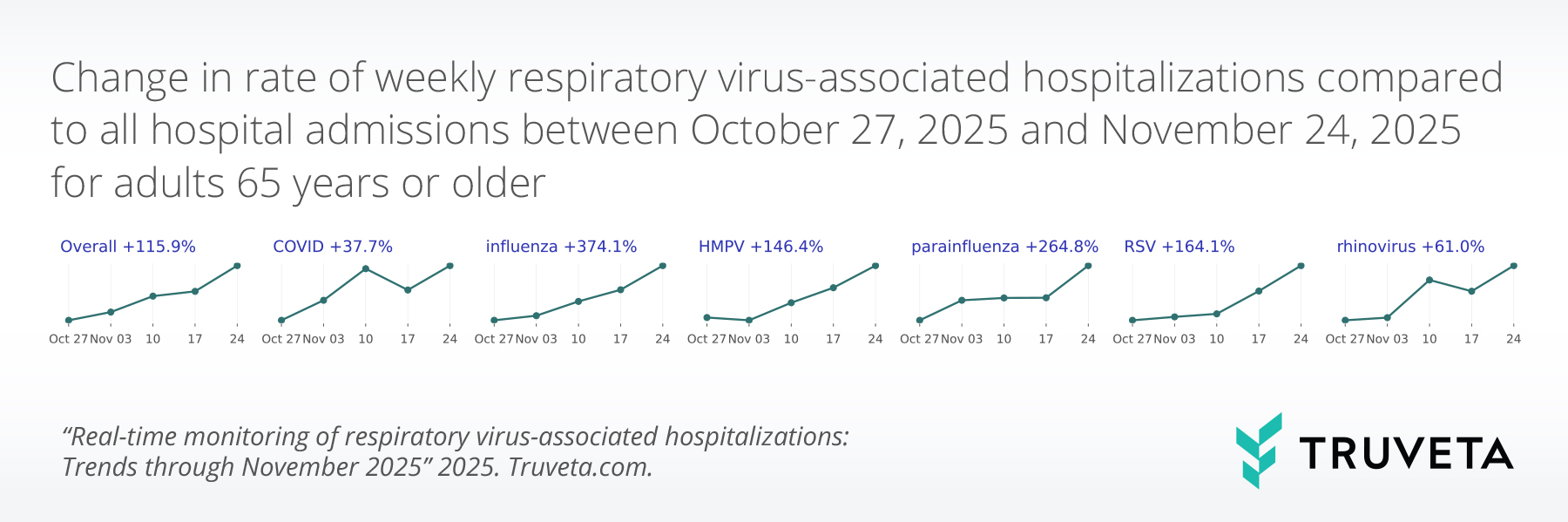
Respiratory virus-associated hospitalizations also increase in adults over the age of 65
Discussion
We will continue to monitor respiratory virus-associated hospitalization overall and for at-risk populations throughout this 2025-2026 respiratory virus season (October 2025 through September 2026).