- Timely receipt of the MMR vaccine for children has been declining since 2021, with just 76.9% of children receiving the MMR vaccine in 2024 on time. The odds of non-vaccination by age two for measles were higher among male children, children in rural areas, White children, and non-Hispanic or Latino children.
- Children who were late in receiving their 2-month and 4-month vaccines—such as DTaP, Hib, IPV, PCV, and Rotavirus—were about seven times more likely to be unvaccinated for measles by age two.
- The strongest predictor of timely MMR vaccination is not demographic—it’s early adherence to the vaccine schedule. Additionally, children attending all recommended well-child visits were significantly more likely to receive MMR by age two.
Vaccination remains one of the most effective public health interventions, dramatically reducing childhood illness and death. Yet, vaccine hesitancy has been growing globally and in the US, a trend accelerated by the COVID-19 pandemic. New research now sheds light on how predictors of MMR (measles-mumps-rubella) vaccination have changed post-pandemic—and what that means for protecting children against preventable disease.
A new Truveta retrospective cohort study of more than 320,000 U.S. children under age two found that fewer children have been receiving their MMR vaccine on time every year since 2021. After rising to 79.9% in 2021, timely MMR coverage fell three percentage points to 76.9% by 2024. This trend reflects nationwide increased susceptibility to measles among children. We have seen these effects play out this year, with over 1,000 measles cases and three deaths reported – the first US measles deaths in a decade.
Key findings: Early delays, long-term consequences
Perhaps the most critical finding from the study is that early vaccination behaviors have a very strong impact on later vaccination outcomes. Children who were late in receiving their 2-month and 4-month vaccines—such as DTaP, Hib, IPV, PCV, and Rotavirus—were up to seven times more likely to miss MMR vaccination entirely by age two. Specifically:
- Late receipt of second-month vaccines was associated with nearly 7-fold higher odds of missing MMR entirely (adjusted odds ratio [aOR] 6.96).
- Late fourth-month vaccination was associated with over a 6-fold increase in odds of missed MMR (aOR 6.16).
These findings underscore the importance of early intervention. When a child begins to fall off the recommended vaccine schedule, even by just a few months, the risk of complete non-vaccination for later vaccines like MMR increases dramatically.
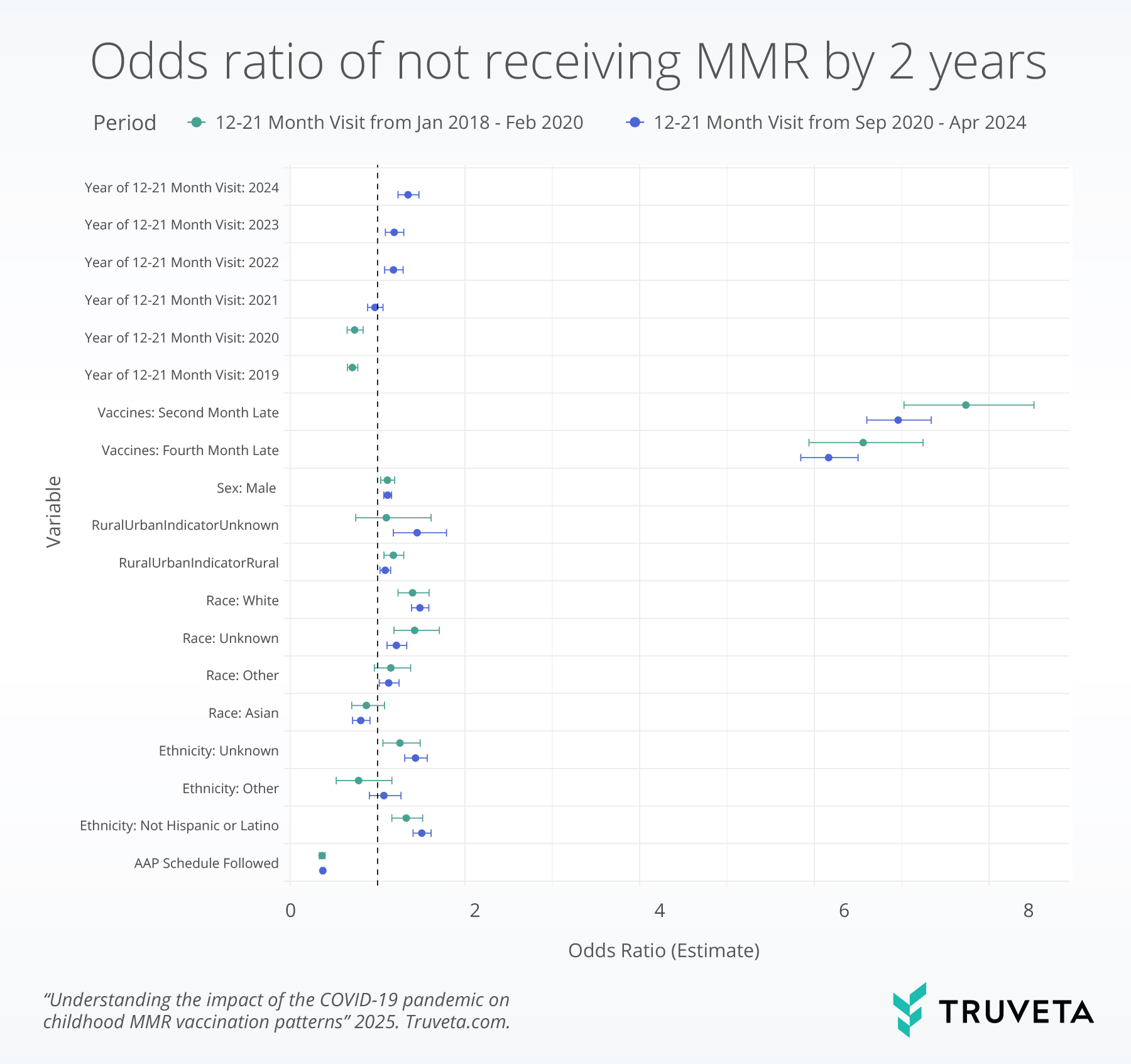
Figure 1. Odds ratios of not receiving any MMR by two years of age vs. receiving any MMR, stratified by 12–21-month visit before or after the COVID-19 pandemic
A changing landscape since COVID-19
The study also found a steady rise in the proportion of children who did not receive any MMR vaccine by age two—increasing from 5.3% in 2020 to 7.7% in 2024. The overall drop in vaccination rates since the pandemic aligns with broader concerns that COVID-19 may have deepened mistrust in vaccines generally.
Demographic factors also played a role. The odds of non-vaccination were higher among:
- Male children
- Children living in rural areas or areas of unknown urbanicity
- White children and those identified as non-Hispanic or Latino
Meanwhile, adherence to the American Academy of Pediatrics (AAP) well-child visit schedule was strongly protective: children attending all recommended visits were significantly more likely to receive timely MMR.
You can read the full study on MedRxiv.
Implications for providers and policy
The strongest predictor of timely MMR vaccination is early adherence to the vaccine schedule. This means pediatricians have a powerful opportunity, and crucial role during the first few months of life to identify and support families at risk of falling behind. Proactive communication, EHR-integrated alerts, and continued parent education may help improve outcomes.
With the resurgence of measles in the U.S., timely vaccination is more important than ever. Amid changing policy and leadership, confusion around the childhood vaccine schedule and insurance coverage of routine vaccines is likely to grow rapidly, which will likely contribute to continued declines in vaccination coverage. Our findings suggest that interventions targeting the earliest stages of a child’s immunization journey may prove to be the most effective strategy for improving MMR coverage and preventing future outbreaks.