Yale School of Medicine, New Haven, CT, Senthil K. Nachimuthu, MD ⊕Truveta, Inc, Bellevue, WA, Brianna M. Goodwin Cartwright, MS ⊕Truveta, Inc, Bellevue, WA, Michael D. Wang, MD ⊕Truveta, Inc, Bellevue, WA
, Charlotte Baker, DrPH MPH CPH ⊕Truveta, Inc, Bellevue, WA, Patricia D. Rodriguez, PhD, MPH ⊕Truveta, Inc, Bellevue, WA, Mackenzie Bogiages ⊕Truveta, Inc, Bellevue, WA, Benjamin M. Althouse, PhD ⊕Truveta, Inc, Bellevue, WA, Information School, University of Washington, Seattle, WA
Department of Biology, New Mexico State University, Las Cruces, NM, Nicholas Stucky, MD PhD ⊕Truveta, Inc, Bellevue, WA
Background
The successful development of multiple COVID-19 vaccines has led to a global vaccination effort to reduce severe COVID-19 infection and mortality. However, the effectiveness of the COVID-19 vaccines wane over time leading to breakthrough infections where vaccinated individuals experience a COVID-19 infection. Here we estimate the risks of breakthrough infection and subsequent hospitalization in individuals with common comorbidities who had completed an initial vaccination series.
Methods
Fully vaccinated was defined as 14 days after one dose of Janssen or 14 days after two mRNA doses at least 17 days apart for Pfizer and 24 days apart for Moderna. The time between doses for Pfizer and Moderna vaccines include a four-day buffer allowance from the CDC.
Additionally, discordant doses (mix and match) were included as fully vaccinated. A booster dose was defined as 14 days following an additional dose, which occurred over 100 days after the most recent vaccination.
Breakthrough infections were defined as a COVID-19 infection for an individual who was either fully vaccinated or fully vaccinated with a booster.
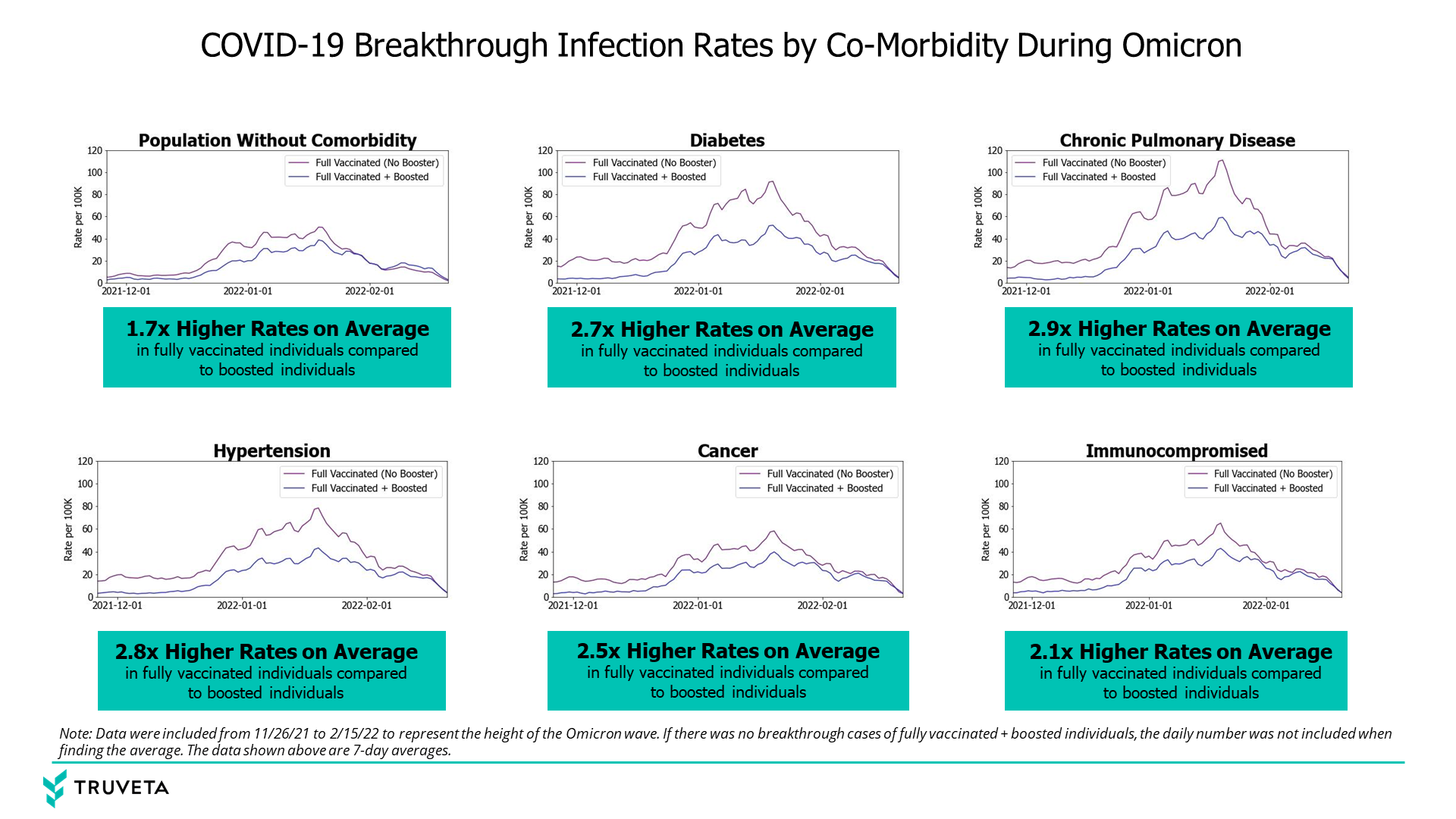
We calculated the fully vaccinated and boosted breakthrough rates over time for people with immunocompromising conditions, diabetes, hypertension, cancer, and chronic pulmonary disease at the time of their first vaccination.
We also calculated these rates for people who did not have any of these co-morbidities. If a person had multiple diseases listed above, they were included in both disease groups. We restricted our analysis to the Omicron wave (November 26, 2021 – February 15, 2022).
We found the average daily ratio of fully vaccinated breakthrough rates to boosted breakthrough rates over the time period to get a rate of increased risk during the Omicron wave.
During days where no breakthrough cases occurred, this daily value was not included in the average.
Results
Of 1,218,630 patients in the Truveta Platform who had completed an initial vaccination sequence between January 1, 2021 and March 31, 2022, 2.85, 3.42, 2.75, and 2.88 percent of patients with CKD, chronic lung disease, diabetes, or are in an immunocompromised state experienced breakthrough infection, respectively, compared to 1.46 percent of the population without any of these four comorbidities. We found an increased risk of breakthrough infection and subsequent hospitalization in individuals with any of the four comorbidities when compared to individuals without these four comorbidities.
Conclusions
Vaccinated individuals with any of the studied comorbidities experienced an increased risk of breakthrough COVID-19 infection and subsequent hospitalizations compared to the people without any of the studied comorbidities. Individuals with immunocompromising conditions and chronic lung disease were most at risk of breakthrough infection, while people with CKD were most at risk of hospitalization following breakthrough infection. Patients with multiple comorbidities have an even greater risk of breakthrough infection or hospitalization compared to patients with none of the studied comorbidities. Individuals with common comorbidities should remain vigilant against infection even if vaccinated.
Read the full peer-reviewed study in Vaccine.