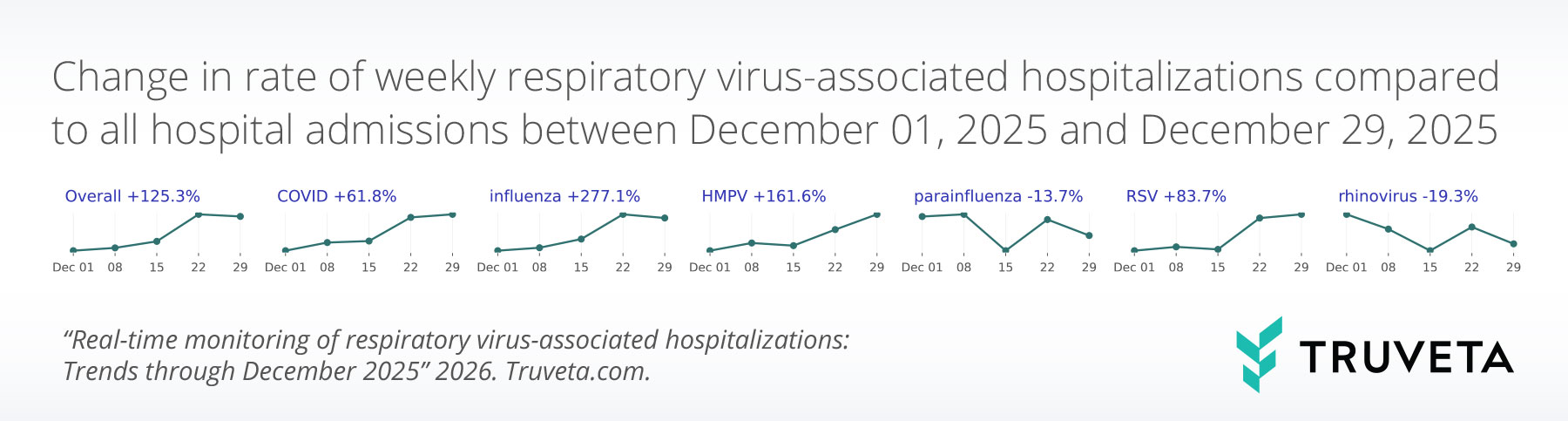
- Respiratory virus–associated hospitalizations increased substantially (+125.3%) in December 2025 and accounted for nearly 7% of all hospitalizations by the last week of the month. This increase was driven primarily by a rise in influenza-associated hospitalizations (+277.1%).
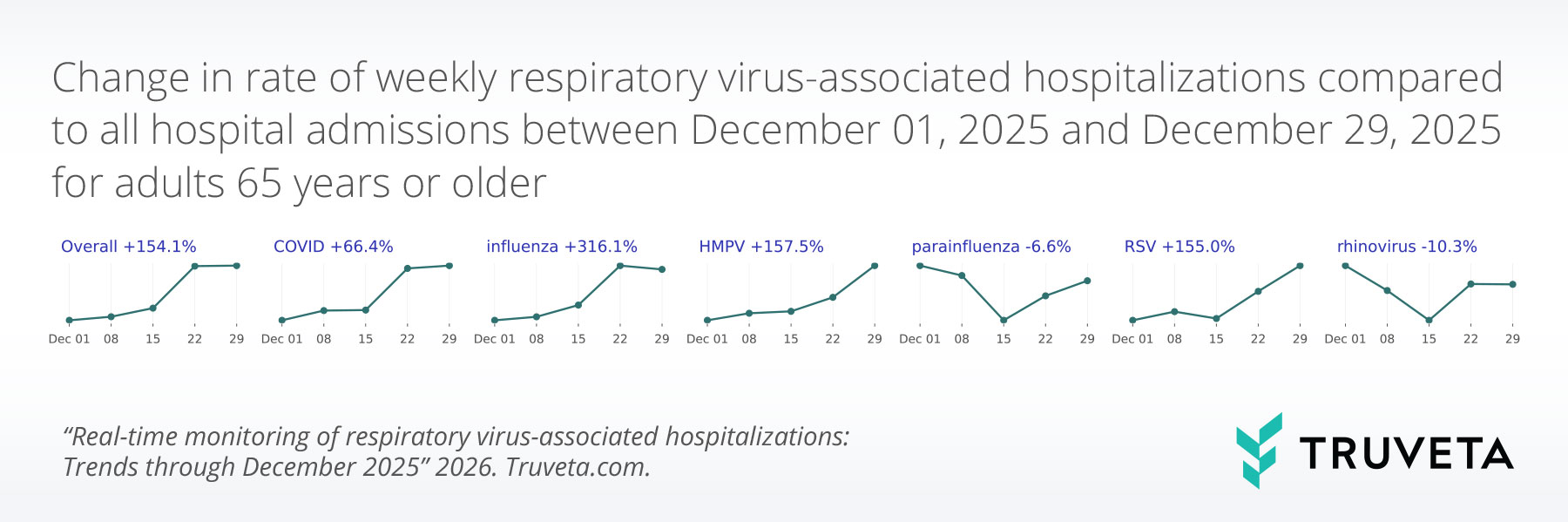
- Among adults aged 65 and older, respiratory virus–associated hospitalizations rose sharply (+154.1%), reaching 9.4% of all hospitalizations by the end of December. Influenza-associated hospitalizations in older adults increased more than fourfold across the month and now account for nearly 6% of hospitalizations in this age group.
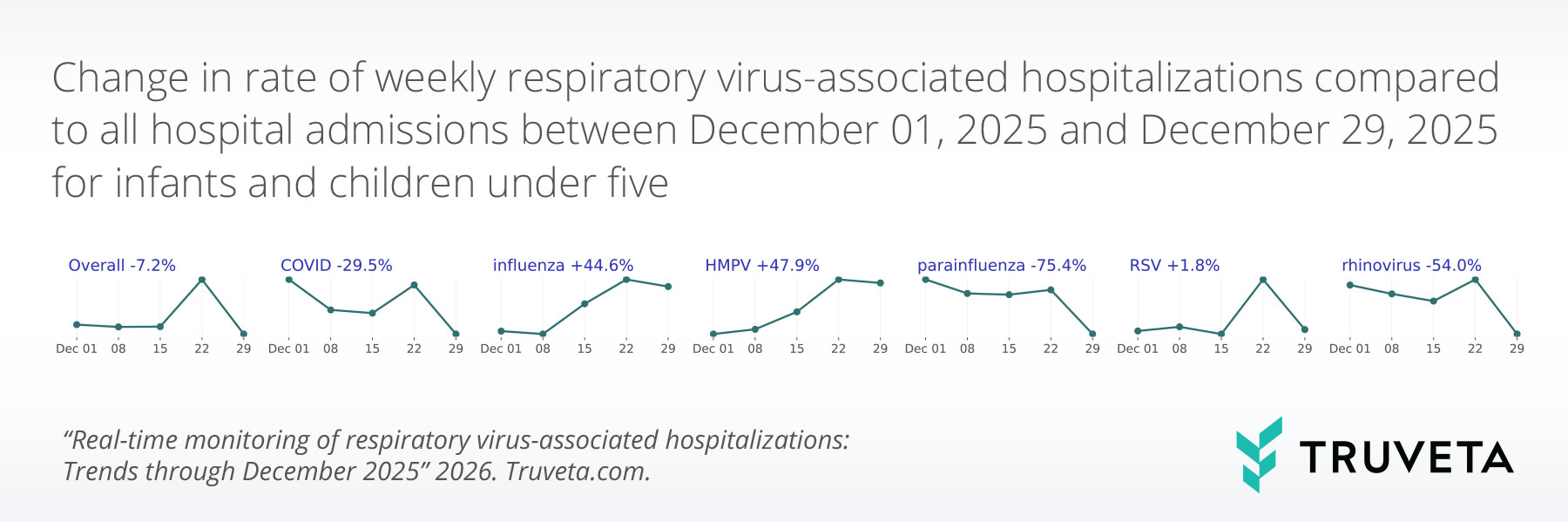
- In children aged 0–4 years, RSV-associated hospitalizations remained the leading cause of respiratory-virus associated hospitalizations (1.7% of all hospitalizations at the end of the month).
Respiratory viruses, including COVID-19, influenza, and respiratory syncytial virus (RSV), continue to contribute to hospitalizations across the United States. Vulnerable populations, such as infants, children, and older adults, are particularly at risk of severe outcomes. Few sources regularly monitor hospitalizations associated with respiratory viruses. Truveta Research has created a respiratory virus monitoring report to supplement the surveillance data provided by the CDC by describing weekly trends in the rate of hospitalizations overall and for each of the six most common respiratory viruses: COVID-19, influenza, human metapneumovirus (HMPV), parainfluenza virus, RSV, and rhinovirus. This information can inform decisions about public health, clinical care, and public policy.
Because Truveta Data provides the most complete, timely, and clean de-identified EHR data, including full patient medical records, notes, and images, linked with closed claims for more than 120 million patients across the US, we can show the latest trends in these respiratory virus-associated hospitalizations, including valuable insight into two at-risk populations: infants and children (age 0-4 years old) and older adults (age 65 and over).
This report provides a snapshot of the key findings with data through December 2025 in the report specific to the overall population across all respiratory viruses, as well as for two high-risk populations: infants and children (age 0-4 years old) and older adults (age 65 and older). For the full analysis—inclusive of demographics, comorbidities, and overall trends in virus-associated hospitalizations and testing across all age groups for each virus—see the complete report with data through January 4, 2026 on MedRxiv.
Key findings: Trends in respiratory virus-associated hospitalizations
Using a subset of Truveta Data, we identified 1,010,216 hospitalizations of 885,367 unique patients who tested positive for a respiratory virus between October 1, 2020 and January 4, 2026.
Overall hospitalization rates increasing substantially
The overall rate of respiratory virus-associated hospitalizations increased substantially in December. By the last week of the month, respiratory virus-associated hospitalizations accounted for 6.9% of all hospitalizations, up from 3.0% at the beginning of December. This represents a 125.3% increase over the month.
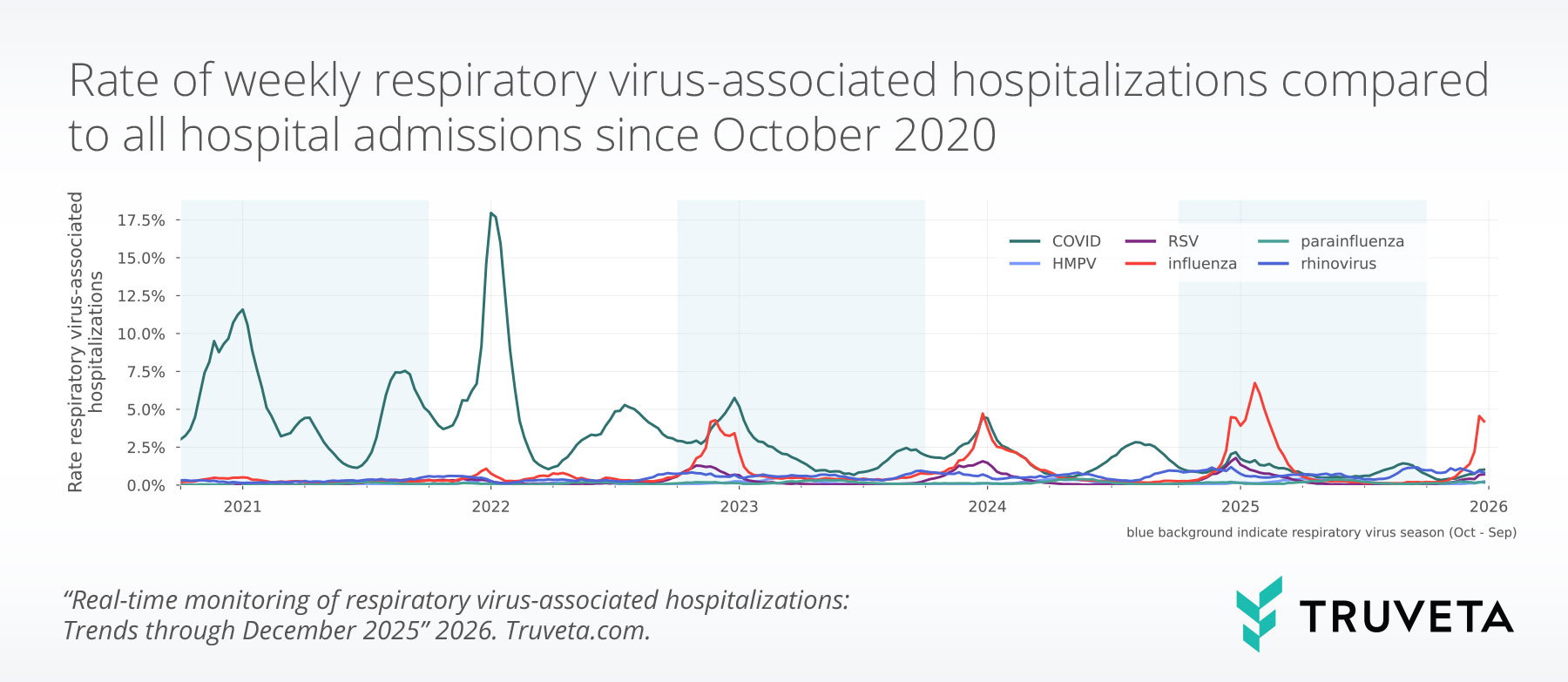
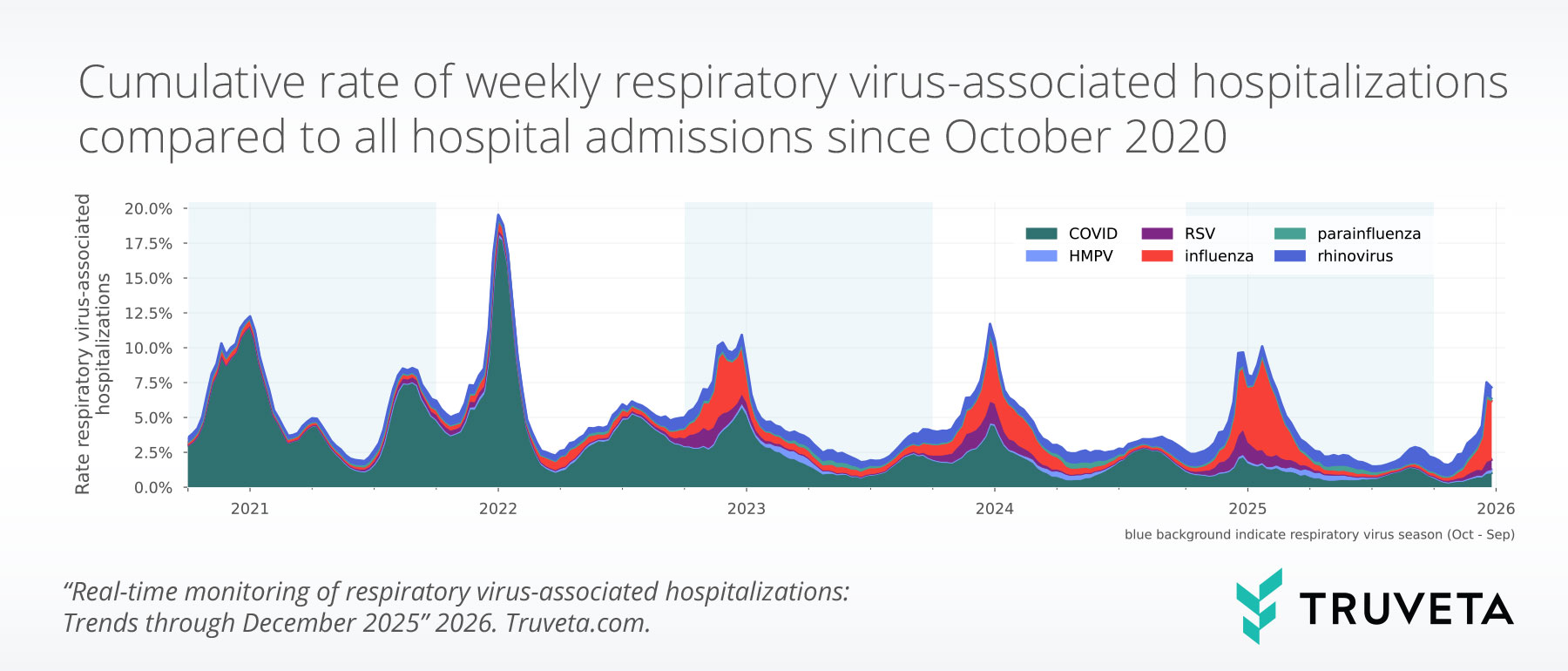
This increase was driven primarily by influenza, with influenza-associated hospitalizations rising from 1.1% to 4.2% of all hospitalizations (+277.1%). COVID- and RSV-associated hospitalizations also increased (+61.8% and +83.7% respectively), while rhinovirus-associated hospitalizations decreased slightly across the month (-19.3%). HMPV- and parainfluenza-associated hospitalizations remained relatively low and stable.
Pediatric respiratory virus-associated hospitalizations remain relatively stable
Among children aged 0–4 years, respiratory virus-associated hospitalizations remained relatively stable throughout December and accounted for 3.6% of all hospitalizations by the end of the month.
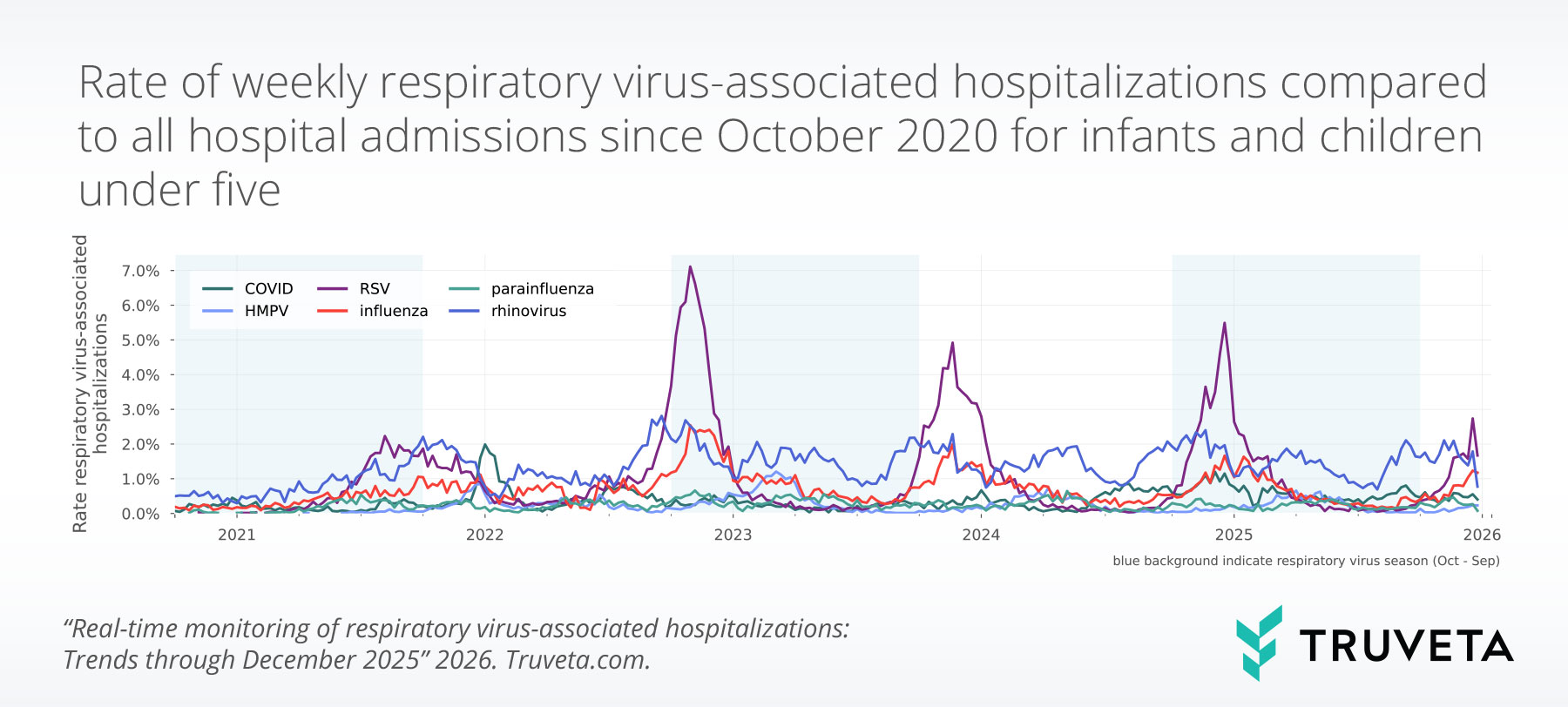
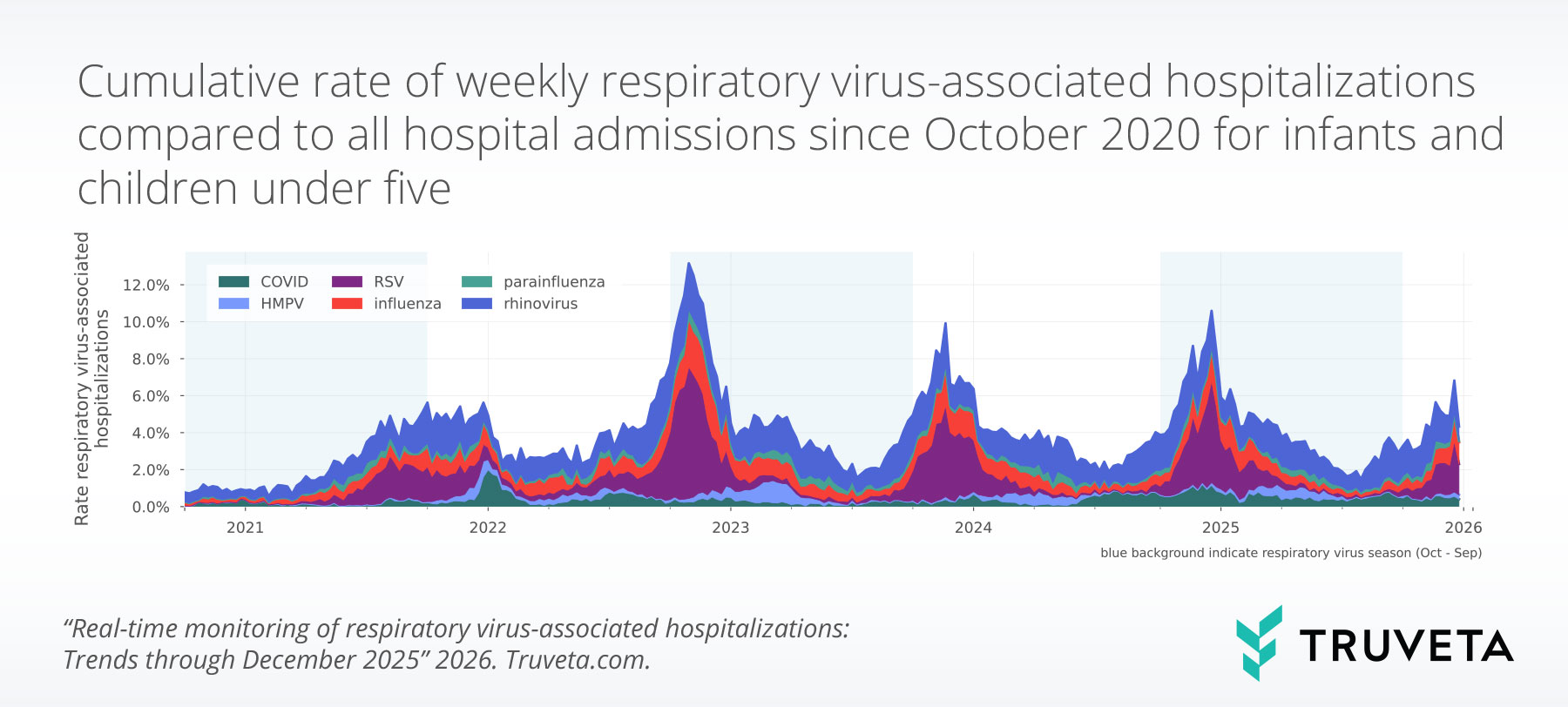
This stability reflects opposing trends, with influenza-associated hospitalizations increasing from 0.8% to 1.2% of all hospitalizations, offset by declines in rhinovirus-, COVID-, and parainfluenza-associated hospitalizations.
Respiratory virus-associated hospitalizations increase sharply in adults over 65
Among adults aged 65 and older, respiratory-virus associated hospitalizations increased sharply to 9.4% of all hospitalizations (+154.1%) in the last week of December.
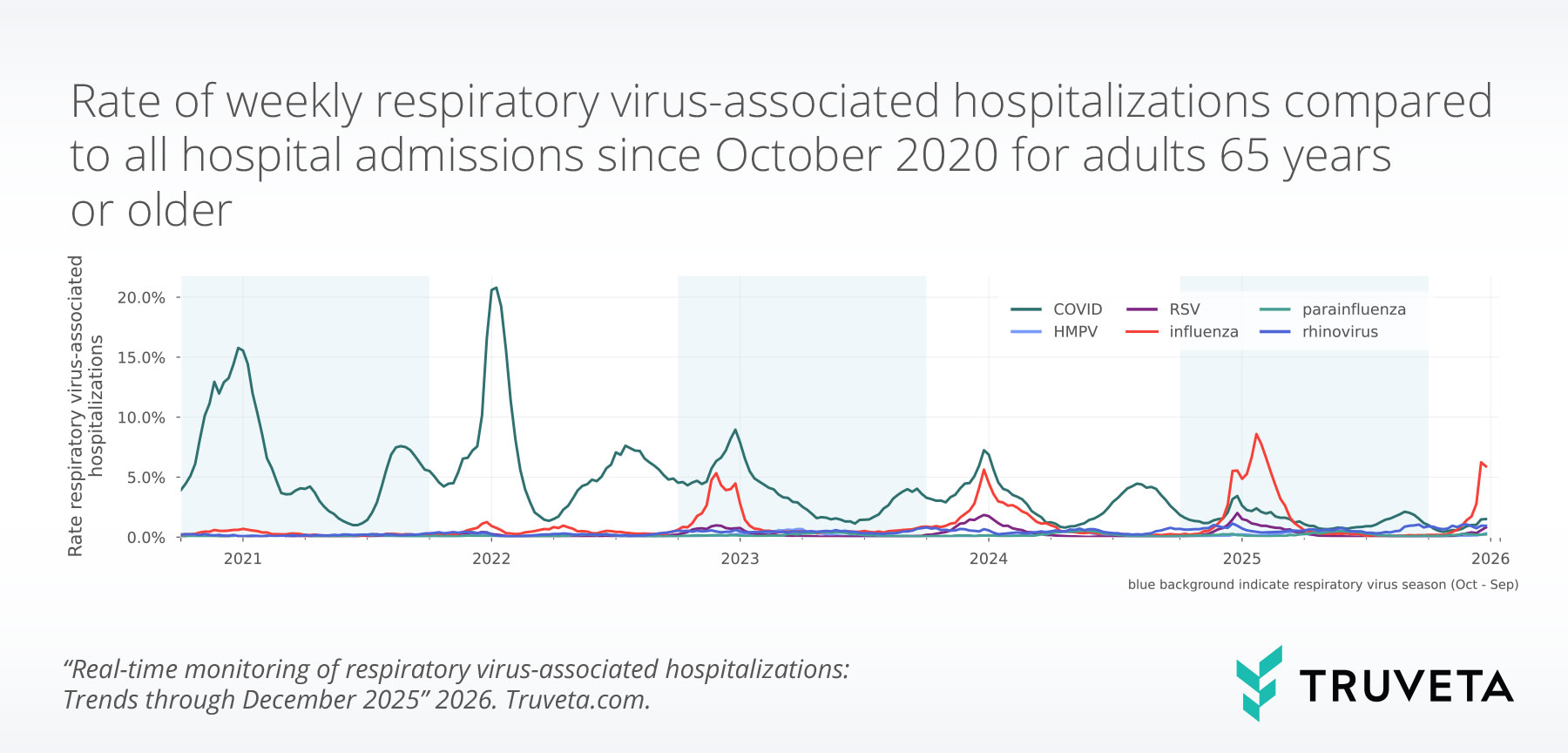
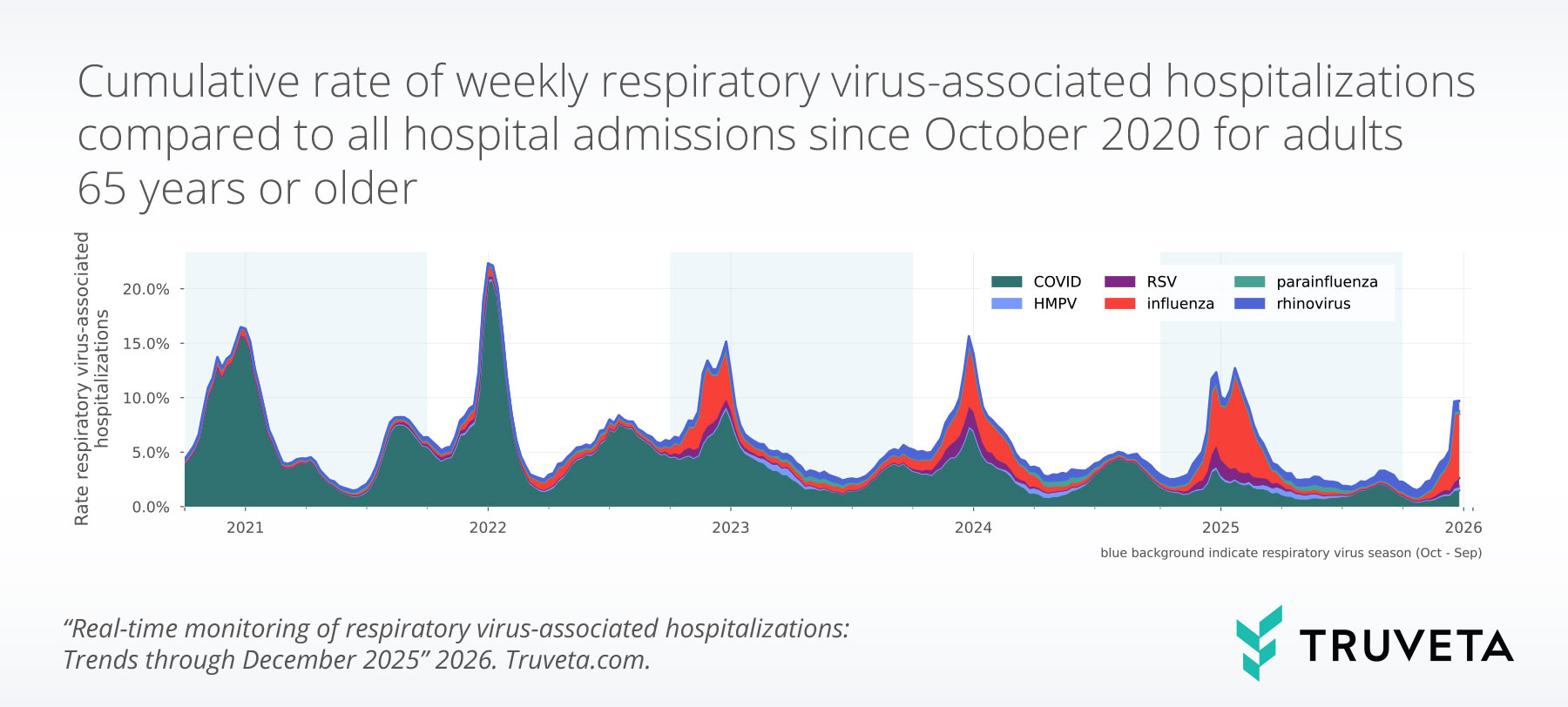
Influenza-associated hospitalizations increased more than fourfold (+316.1%) and were the primary driver of this increase. COVID-, RSV-, and HMPV-associated hospitalizations also rose (+66.4%, +155.0%, and +157.5%, respectively), while rhinovirus-associated hospitalizations declined slightly. Parainfluenza-associated hospitalizations remained low and stable.
Overall, these findings indicate a substantial increase in respiratory virus associated hospitalizations among older adults across December, driven primarily by influenza, with additional increases also observed for COVID, RSV, and HMPV.
Discussion
It is important for public health experts and clinical providers to understand the trends in these infections to inform decisions about public health, clinical care, and public policy. Connecting population-level trends with granular clinical information can be very useful to understand which populations are most impacted and may require additional support.
We will continue to monitor respiratory virus-associated hospitalization overall and for at-risk populations throughout this 2025-2026 respiratory virus season (October 2025 through September 2026).