This month, in our Meet the MDs series, we’re featuring Michael Wang, MD. Mike is a clinical informaticist and has worked with Truveta for a little over a year.
What is a clinical informaticist?
You should ask 100 clinical informaticists and let me know; even my own definition changes over time. For me right now, it’s taking information and wiring it to the right place for people to consume it at the right time. That’s not necessarily digital information either. Especially in the clinical world, a lot of it is paper, analog pictures, or stories known only to patients or providers. It’s about getting the most relevant bits of information to the people who need it to make a decision.
Can you tell me a little bit about your background?
I grew up in Orange County, CA, went to college in Boston, and medical school in Chicago. I did my internal medicine training and clinical informatics training in San Francisco, where I still live. I did a short stint as a software developer before medical school, but once you start practicing medicine, you don’t want to stop. I still practice at about 30%.
What inspired you to get into medicine and become a doctor?
My dad was a Kaiser physician, a gastroenterologist who was also involved in leadership, so in the back of my mind, I always thought I could be a doctor. My dad has a public health degree and is always talking about policy and population health. With this in mind, I always coded growing up, so I built a database for my dad in 1997 as a high school student, probably my first foray into building clinical data warehouses. Other manifestations of this population-focused interest were data mining (the old term for big data) and genome sequencing, but I ultimately decided to go into medicine to be on the receiving end of all this data since, in the early 2000s, it seemed like the place with the most work to be done. It didn’t hurt that my parents had clearly planned this all out since my first two initials were already MD.
What brought you to Truveta?
I was trying to do three careers at once. I was practicing medicine, I was pursuing academia, and I was involved in product at a startup. I decided that was too much and I wanted to work for one company that would allow me to do both data and product. There’s a lot of startups out there that have funding and a product, but very little healthcare data. When I saw an article about Truveta describing the vast volume and diversity Truveta was being founded with, it seemed like an obvious fit, so I applied. Dating back to my days in genetics, it’s always been a dream of mine to conduct research on millions of patients across both their clinical and -omics data; it’s something Truveta is well positioned to make a reality.
Data quality in particular has always been a particular interest of mine; it’s not about generating 99% pure gold all the time. It’s about generating whatever quality gold you can generate and making sure you put a label on it with how pure it is. As long as people know how pure it is, they can figure out how to use it. I joke that at the end of the day, our researchers are like jewelers, consuming all these things that we’ve extracted; they just need to know what they have so they can create the best finished product from it.
What does Truveta’s vision of saving lives with data mean to you?
I spent two years trying to collate a dataset from three different hospitals for around 3,500 patients with COVID. Early in my work here, I got access to our research platform, I did a two-minute query, and immediately got around 15 million COVID patients. The scale Truveta’s data brings to the table can really transform the types of questions researchers can answer. I’ve struggled my entire academic career to create generalizable insights across multiple clinical settings and we actually have the data where it’s a one-stop shop. We have the potential to accelerate insights from years to hours.
How does health equity factor into the work you do?
Truveta will have unparalleled data to study minority populations. As an example, borrowing from my genetics past, when a person has a heart attack and gets a stent placed, they routinely receive Plavix, which improves overall outcomes. However, people with a certain genetic mutation in a gene called CYP2C19 have worse outcomes than those who don’t have the mutation and do better on alternative medications, but this genetic testing is not yet standard of care in patients get prescribed Plavix. The fact that this testing is not standard disproportionately affects minority patients. It has been estimated that these mutations occur in ~2% of white patients, but in ~4% of Black patients and a higher percentage of Asian patients (~14% in Chinese patients). Despite these phenomena being described since 2010, it’s only this year (2022) that we are starting to see large-scale, real-world data results. Having a large-scale data platform like Truveta that is intimately tied to real-time clinical data can significantly accelerate bench to bedside insights like this in the future, especially for situations like that with Plavix where minority populations, defined by race, genetic factors, geography, care delivery setting (rural vs. urban), are unequally affected. Meanwhile, our collaboration with LexisNexis will also offer an unprecedented set of patient characteristics to leverage for studying health inequity. These factors together really position Truveta well to address both health equity and personalized medicine.
What do you like to do outside the office?
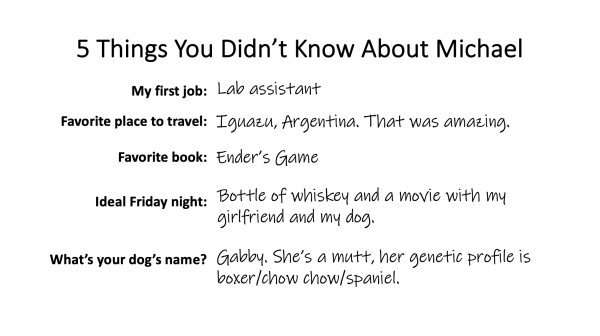
These days, I play a decent amount of tennis when I’m not working (often with another clinical informaticist Dr. Ryan Lee). I have a dog that I try to keep entertained. Thanks to our designers, she is on the board of Truveta for Dogs.

Michael’s dog, Gabby
What’s your favorite part about working at Truveta?
When I look for jobs, it’s usually people first and the mission is a close second. Truveta has both in spades.
What are you looking forward to next?
I’m still pretty interested in teaching and education, especially around informatics. I’m running our program for visiting clinical informatics fellows and still engage with ACIF, the national society for clinical informatics fellows, which I helped start with a few friends some years ago. If only there wasn’t so much else to do!