This post kicks off our new series, Truveta experts— a spotlight on the data scientists, researchers, clinicians, and analysts working behind the scenes to drive healthcare research forward with real-world data.
Our first contributor is Mantas Dmukauskas, PhD, a research analyst on Truveta’s Partner Research & Success team. Mantas holds a PhD in physics from Vilnius University and previously served as a postdoctoral fellow at the National Cancer Institute, where he led projects using cancer registries and insurance claims data. After partnering with Truveta on a research project exploring Mantas joined full-time to help more researchers unlock insights from real-world clinical data.
His latest insight from Truveta Data was inspired by his wife—an oral medicine specialist and reveals a disconnect in the treatment of a rare but life-altering condition: trigeminal neuralgia.
Trigeminal neuralgia: Still under-treated in real-world practice
Trigeminal neuralgia (TN) is a chronic neuropathic pain disorder defined by sudden, stabbing pain across one side of the face—often triggered by simple actions like talking or brushing teeth. (Mantas’ wife, a doctor in oral medicine, often sees TN patients in her practice that have been referred to her with a misdiagnosis and lack of awareness of their treatment options.) The pain from TN is so intense that it is often compared to an electric shock.
While rare (affecting ~150,000 people annually in the US), TN’s impact on quality of life is profound.
First-line therapies are clear. But are they being used?
Clinical guidelines recommend carbamazepine and oxcarbazepine as first-line therapies. These medications have been proven to reduce TN pain, are low cost, and can be taken orally, yet real-world data shows these treatments may be underused.
What Truveta Data shows
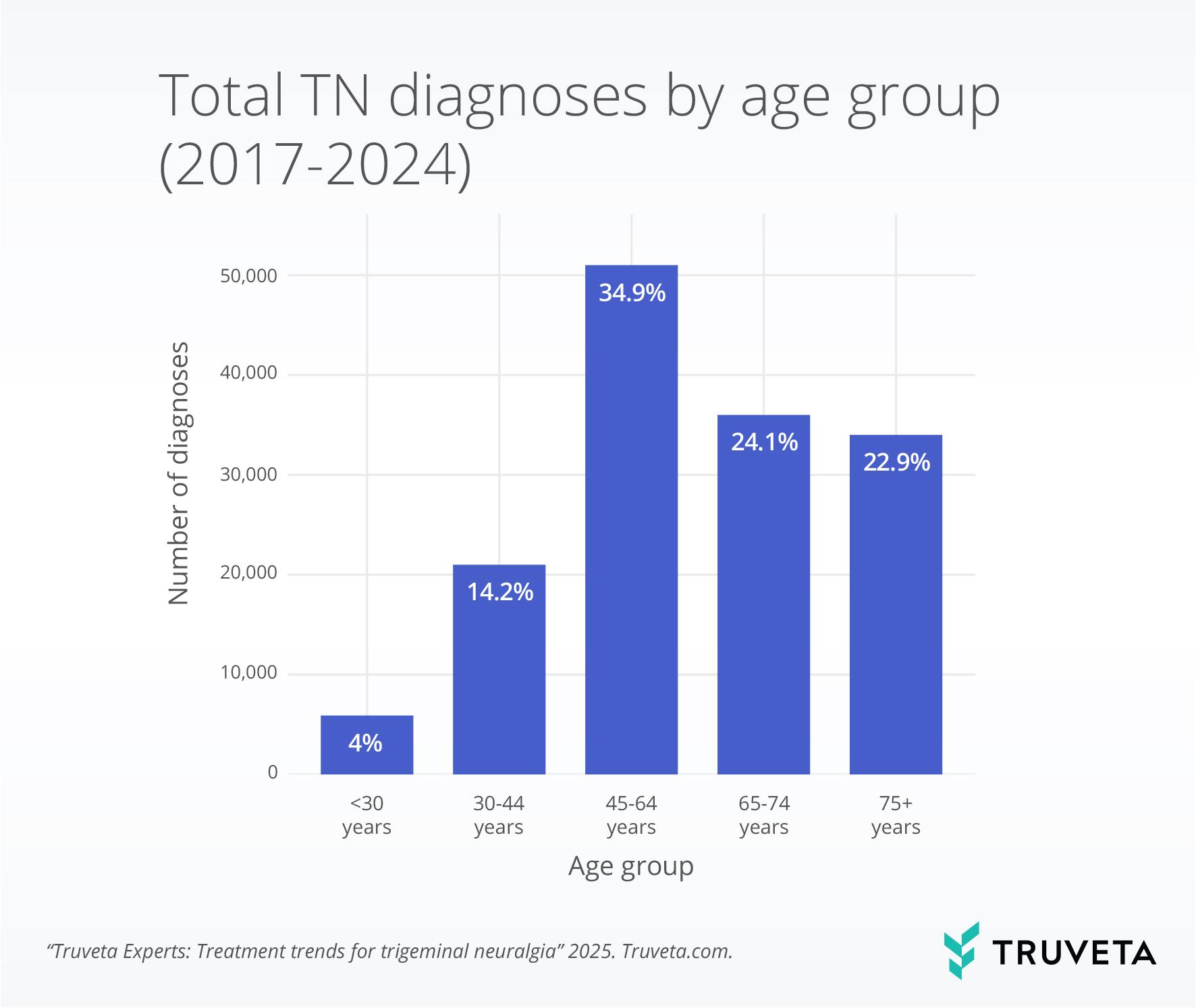
To better understand how many patients diagnosed with TN are receiving first-line treatment, Mantas was able to quickly build a population of over 134,000 patients who were diagnosed with TN between 2017 and 2024.
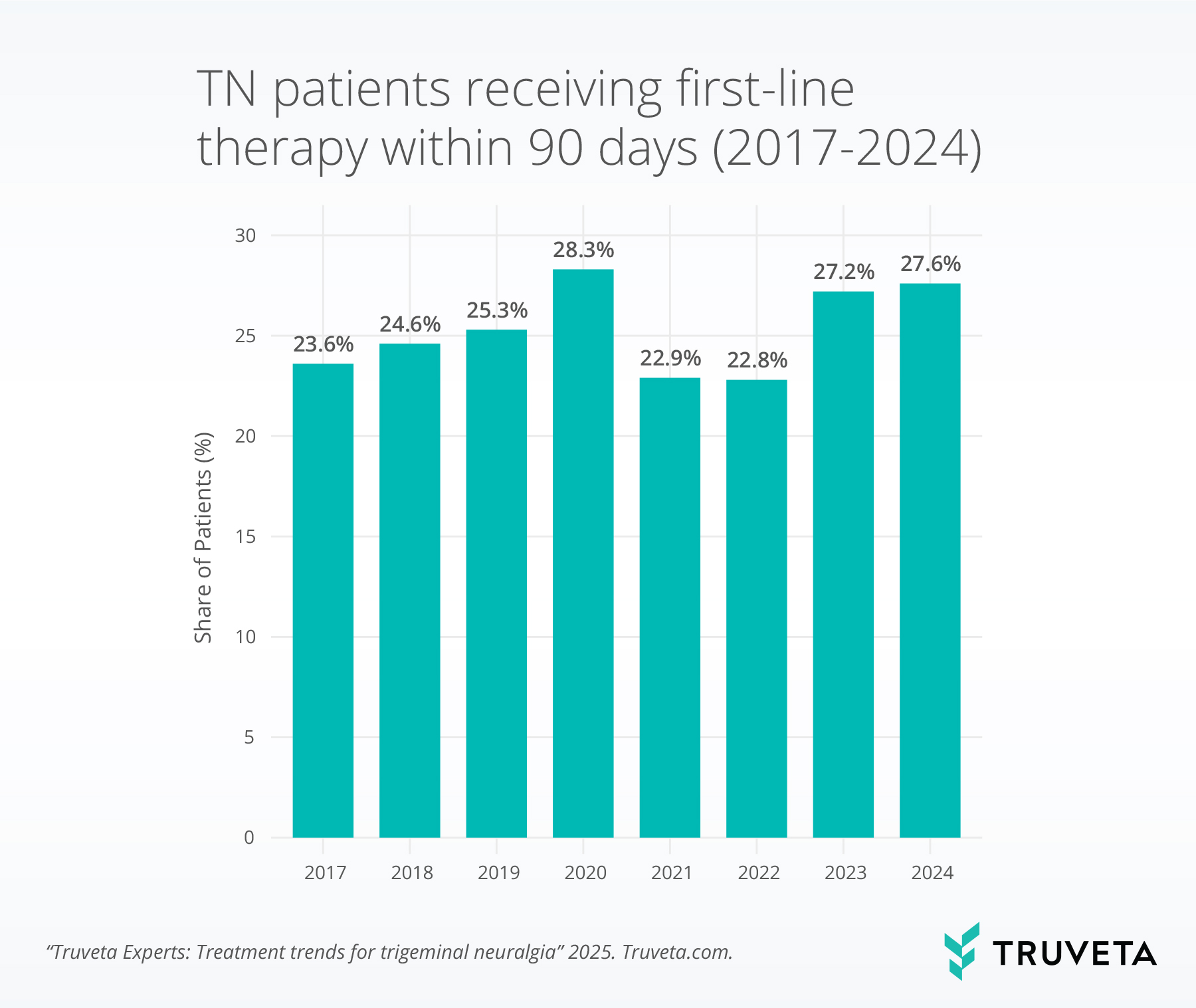
Here’s what he observed for first-line therapy initiated within 90 days:
- In 2017, only ~24 % of diagnosed patients started first-line treatment within 90 days.
- By 2020, that number rose to just ~28%, and has stagnated since.
- 60% of diagnoses occurred in adults aged 45–74.
- Majority of diagnoses (65%) occurred in women, reflective of the literature.
Insight
Despite strong evidence and clinical recommendations, the adoption of first-line TN therapy remains far below optimal —and it’s not improving over time.
This raises important questions for clinical and pharma teams alike:
- Are there barriers to diagnosis or prescription?
- Do providers lack confidence in these therapies?
- Are patients discontinuing due to side effects, cost, or other factors?
Real-world data like Truveta’s can help answer those questions—and guide better outcomes.
Opportunities for further research
- Alternative treatments: Emerging therapies like Botox show promise in clinical studies, though not yet FDA-approved for TN.
- Root cause analysis: MRI scans may help identify structural causes like multiple sclerosis or tumors. With the largest collection of medical images integrated with real-world data, Truveta offers a unique opportunity to study diagnostic patterns at scale.
Stay tuned for more Truveta Experts, where we share real-world evidence and analysis from the people powering Truveta’s mission.
See how Truveta Data can accelerate your next study—Request a customized demo today
