Just last week marked the two-year anniversary of the first case of COVID-19 in the United States, discovered by our health system member Providence. It’s hard to believe that it’s been two years, and just this past month we’ve experienced the highest number of daily cases at any point in the pandemic.
If the pandemic has taught us anything, it’s that we still have so much to learn. With the emergence of the Delta and Omicron variants in 2021, COVID-19 has created ongoing challenges for researchers– and the healthcare system is more strained than ever. Collectively, the world still lacks the data needed to learn quickly about COVID-19 as it evolves, not to mention thousands of other conditions.
That need is why 20 health systems have come together to form Truveta with the vision of saving lives with data. By combining de-identified patient data representing more than 16 percent of clinical care across the U.S., the Truveta Platform enables researchers to find cures faster, empower every clinician to be an expert, and help families make the most informed decisions about their care.
New COVID-19 hospitalization insights
With the spike in COVID-19 cases around the world, there has been much interest in whether the Omicron variant is more or less severe than the Delta variant. We queried a subset of data within the Truveta Platform to see what we could learn.
By exploring positive COVID-19 cases and hospitalizations between May 1, 2021 and January 6, 2022 in the Truveta Platform, we compared trends across the Delta and Omicron spikes in the U.S. Hospitalizations are a good indicator of disease severity, so we focused on trends in COVID-19 positive hospitalizations across three populations:
- Unvaccinated: Individuals who at the time of infection had not received a Covid-19 vaccine,
- Vaccinated Breakthrough: Individuals who were infected 14+ days after being fully vaccinated. Fully vaccinated was defined as two mRNA vaccine (Moderna or Pfizer) 21+ days apart or a single dose of the Janssen vaccine, and
- Boosted Breakthroughs: Individuals who were infected 14 + days after receiving a booster vaccine (booster vaccine is defined as receiving a vaccine 100+ days after being fully vaccinated.
Note: Our graphs combined vaccinated and boosted breakthrough cases into a single line.
By exploring over 175,000 positive COVID-19 cases and more than 24,000 hospitalizations, we found some interesting insights:
- Percentage of people with COVID-19 who were hospitalized is stabilizing and even decreasing with Omicron: Although we see increases in the number of COVID-19 cases and hospitalizations in both groups over the last month, the percentage of people with COVID-19 who were hospitalized has only mildly fluctuated since August 2021 and has decreased in December.
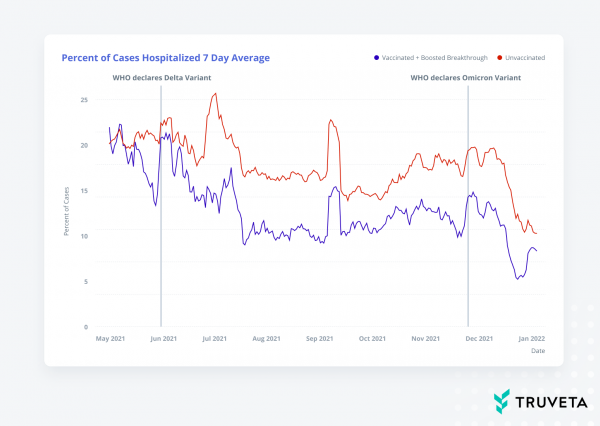
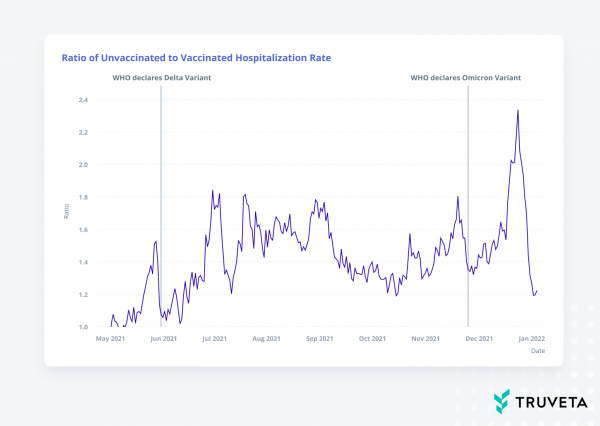
- Higher percentage of hospitalizations for unvaccinated patients, especially with Omicron: For the entire period, the percentage of hospitalized cases was higher in the unvaccinated population than the vaccinated population. The percentage of unvaccinated individuals hospitalized approached two and a half times that of the percentage of fully vaccinated and boosted individuals hospitalized in late December.
- Increased breakthrough cases with Omicron: The insights from these data on case counts are consistent with other reports demonstrating increased cases across vaccination status during the uptick of the Omicron wave (December 2021-January 2022).
In addition to hospitalizations, there’s so much more we need to study as we come out of this pandemic and prepare for future pandemics. We need mortality data from outside the hospital setting to better prevent death, especially since only one-third of deaths happen in a hospital. We need to understand why people of color are disproportionately impacted by COVID-19, not to mention many other conditions. What social factors are at play that we can study and address? What other factors are impacting care, which might only be understood by having a more longitudinal view of a patient’s journey?
These are questions we must explore if we’re going to improve patient lives, and electronic health records only contain some of the answers. We recently announced a partnership with LexisNexis Risk Solutions to incorporate critical mortality, socioeconomic, and medical insurance claims into the Truveta Platform to augment the clinical care data so we can answer those questions to advance research and improve outcomes.
Today’s insights are an important part of our journey and learning. We are excited to see what else we can learn as we incorporate more data and involve more researchers. Imagine the answers we can find together.
