Sign up for a free account to read full studies, with full transparency into methods and results, and experience the power of Truveta Studio
Authors: Truveta Research ⊕Truveta, Inc, Bellevue, WA
Date: March 6, 2024
Abstract
Background
Aortic stenosis prevalence and severity increase with age. Commonly diagnosed with an echocardiogram and staged according to progression, stages are rarely well captured in traditional EHR and claims data. However, the stage of aortic stenosis progression is important for treatment decisions. Truveta Data contains structured data extracted from echocardiogram notes to enable the study of aortic stenosis progression.
The objective of this study was to classify aortic stenosis severity using the data extracted from echocardiogram notes and explore the potential disparities in the types of treatments and time to treatment for those with aortic stenosis.
Methods
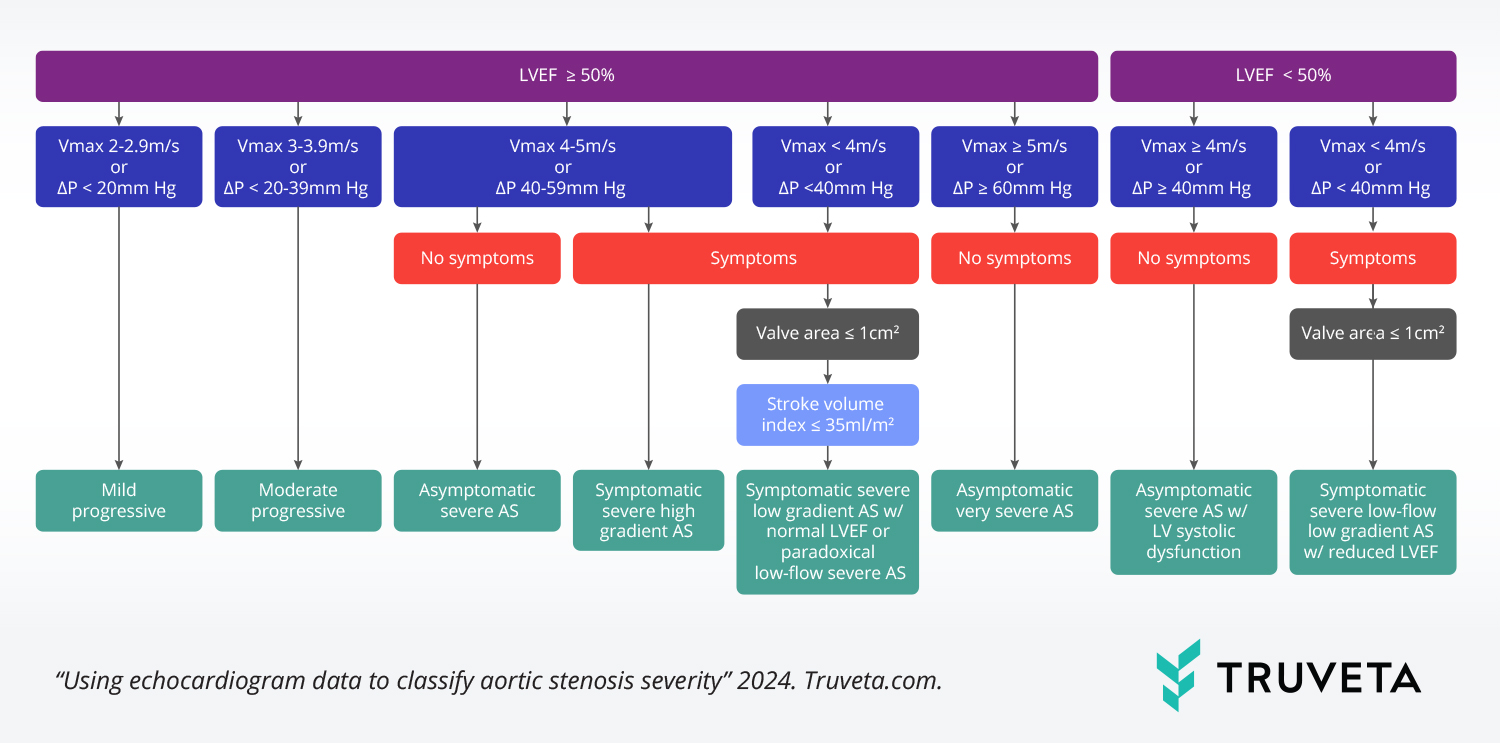
People were included if they had an echocardiogram with a measurement for at least one of the five hemodynamics variables used to classify aortic stenosis severity. Patients were classified as having symptoms of heart failure, angina, or syncope/presyncope prior to the echocardiogram. Hemodynamic variables and symptom data were used to classify eight types of aortic stenosis according to the 2020 American Heart Association guidelines.
We describe the population of people with aortic stenosis by severity. Further, we identified people with four procedures (TAVR, balloon aortic valvuloplasty, SAVR, or aortic value repair procedure). We describe differences in the populations who received each procedure and the time to procedure by demographics and social drivers of health (SDOH) factors.
Results
We identified 485,509 people with echocardiograms classified as aortic stenosis; the largest group was classified as having mild aortic stenosis (82.7%).
We found more than 11,000 people with aortic stenosis and subsequent procedures. Higher rates of TAVR procedures were seen amongst older patients and higher balloon valvuloplasty procedures for patients residing in rural areas, compared to urban areas. There was decreased time between echocardiogram and TAVR procedure with increasing aortic stenosis severity. We also found decreased average time to TAVR for patients who live in an urban setting (compared to rural), for patients with increased individual income (amongst patients who made more than $35,000), and for patients with more familial support (measured by distance to closest relative).
Discussion
We used data extracted from clinical notes to classify aortic stenosis severity and track subsequent echocardiograms, procedures, and disease progression over time. We found TAVR procedures to be performed at higher rates in patients over 65 years of age, consistent with estimates of operative risk and recommendations in these populations. We also found an increased percentage of balloon valvuloplasty in patients residing in rural areas, as well as the longer period between echocardiogram and TAVR in this group. Additional research is required to understand what may be driving these trends and if there are differences in subsequent outcomes.
Sign up for a free account to read this full study, with full transparency into methods and results, and experience the power of Truveta Studio