In this Truveta experts analysis, Amy Sullivan, MS examines real-world antidepressant prescribing episodes using linked electronic health record (EHR) and closed claims data from more than 14.5 million individuals. The analysis characterizes the duration, recurrence, and continuity of antidepressant prescribing across age groups and drug classes, focusing on observed treatment patterns rather than clinical outcomes.
Key points
- Nearly half (46%) of individuals had a single observed antidepressant prescribing episode, while 54% experienced multiple episodes over time—highlighting the episodic nature of antidepressant use in real-world care.
- Prescribing duration varied by age, with older adults more likely to have shorter episodes and younger adults more likely to experience episodes lasting longer than six or twelve months.
- Patterns also differed by drug class: although SSRIs accounted for the largest share of prescriptions, SNRIs and TCAs were more frequently associated with longer continuous prescribing episodes.
Antidepressants are among the most commonly prescribed medications in the United States and are used across a range of clinical indications, including—but not limited to—depression. While clinical trials typically evaluate antidepressant use over relatively short periods (often 8–12 weeks), far less is known about how antidepressant prescribing unfolds over time in real-world care.
Understanding patterns of prescribing continuity and recurrence can provide important context for clinicians, researchers, and policymakers. In particular, real-world data can help illuminate how long prescribing episodes tend to persist, how frequently individuals experience multiple episodes, and whether these patterns differ across demographic groups or antidepressant drug classes.
Using linked electronic health record (EHR) and closed claims data from Truveta, this analysis characterizes antidepressant prescribing episodes—including their duration and recurrence—across age, sex, and drug class. This work focuses on observed prescribing behavior rather than confirmed diagnoses or treatment effectiveness.
Methods
Using linked EHR and closed claims data, patients with at least one recorded antidepressant prescription or pharmacy claim were identified between January 1, 2016, and October 31, 2025. Five commonly prescribed antidepressant drug classes were included: selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants (TCAs), and atypical antidepressants.
Medication records from EHRs and pharmacy claims were combined at the patient level. For each drug class, prescribing episodes were defined based on the timing of observed prescriptions. An episode began on the first recorded prescription date for a given drug class and was considered continuous unless there was a gap of more than 90 days or a switch to a different antidepressant class.
Episode duration was calculated as the time between episode start and end dates based on observed prescribing activity; prescription days supplied were not incorporated. The number of prescribing episodes and the duration of the first observed episode were summarized per patient. Results were stratified by age, sex, and antidepressant drug class. This analysis was descriptive in nature and reflects observed treatment patterns within Truveta Data.
Results
Over 14.5 million individuals (N = 14,540,270) with at least one recorded antidepressant prescription or pharmacy claim were included.
Nearly half of individuals (46%) had a single observed prescribing episode, while the remainder experienced multiple episodes over time: 18% had two episodes, 10% had three episodes, 6% had four episodes, and 20% had five or more episodes. This distribution highlights the episodic nature of antidepressant prescribing in real-world care.
Prescribing episode duration by age
To improve interpretability, the duration of the first observed antidepressant prescribing episode was grouped into clinically intuitive categories (<90 days, 3–6 months, 6–12 months, and >12 months).
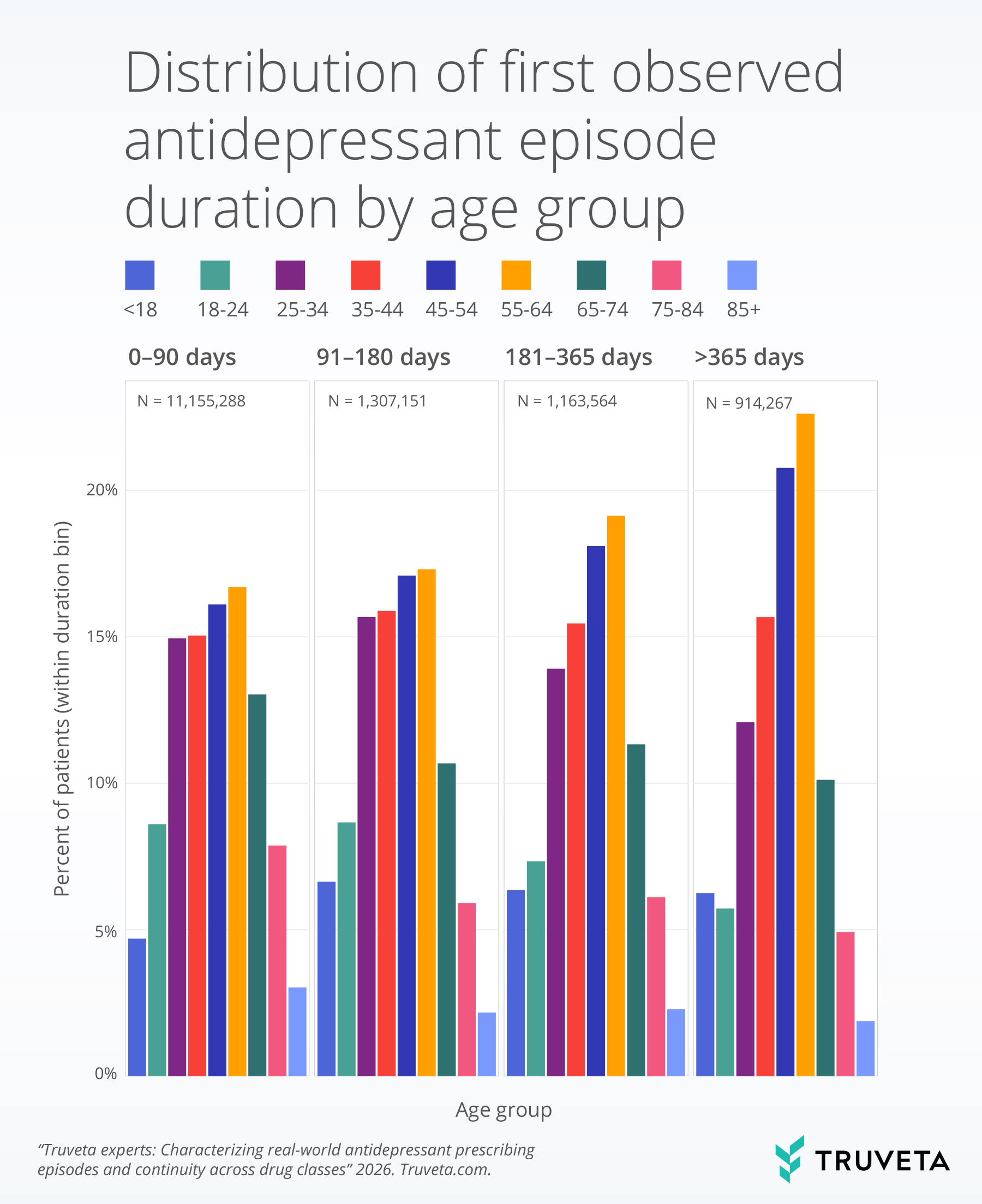
Across age groups, shorter prescribing episodes were more common among older adults, while younger adults more frequently experienced longer continuous episodes extending beyond six or twelve months.
Prescribing episode duration by drug class
When stratified by antidepressant drug class, differences in episode duration were also observed.
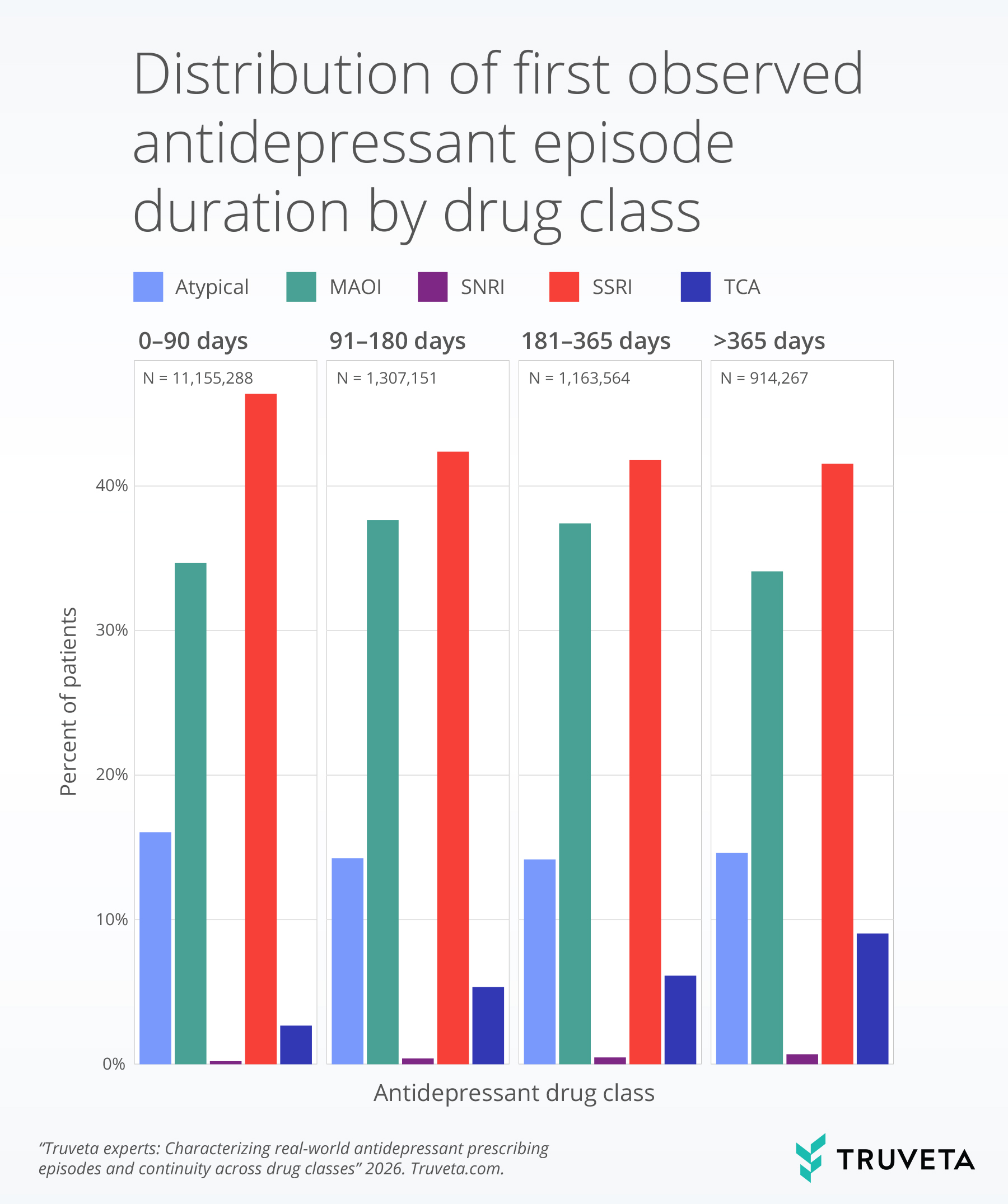
While SSRIs represented the largest proportion of prescribing episodes overall, SNRIs and TCAs were more frequently associated with longer continuous episodes, despite representing smaller patient subgroups.
Discussion
In this large, descriptive analysis, antidepressant prescribing in real-world care was frequently episodic, with many patients experiencing multiple prescribing episodes over time. Nearly half of patients had more than one observed treatment episode, highlighting the dynamic nature of antidepressant use beyond the short, fixed durations typically studied in clinical trials.
Prescribing episode duration varied systematically by age and drug class. Older age groups were more likely to experience shorter prescribing episodes, while certain drug classes were associated with longer periods of continuity. Notably, these findings reflect prescribing behavior captured in EHR and claims data rather than underlying diagnoses, treatment adherence, or clinical outcomes. These patterns suggest that real-world antidepressant use reflects a combination of clinical decision-making, patient characteristics, and treatment tolerability that may differ meaningfully across populations.
Together, these results demonstrate how linked EHR and claims data can be used to characterize real-world medication use at scale, providing insights into continuity, recurrence, and variation that are difficult to capture through trials alone.
This analysis has limitations. Episode definitions were based on observed prescription timing and did not incorporate prescription days supplied or refill adherence. Additionally, the first observed episode and maximum number of episodes reflect what is captured within Truveta Data rather than complete lifetime prescribing histories. Future analyses incorporating days supplied, refill patterns, or indication-specific cohorts may provide deeper insight into treatment persistence, comorbidities, and longer-term outcomes.
These are preliminary research findings and not peer reviewed. Data are regularly updating. These findings are consistent with data accessed in January 2026.
Meet the expert
Amy Sullivan, MS is a data scientist on Truveta’s partner research and success team specializing in biostatistics, with over a decade of experience across areas including real-world data analysis, genomics, life science research and development, and clinical trials across various life science companies.
See how Truveta Data can accelerate your next study—Request a customized demo today.
Explore more in this series:
Treatment trends for trigeminal neuralgia
Fireworks during the fourth of July
Real-world trends in Rituxan biosimilar adoption
Sudden cardiac arrest and arrhythmia among patients with chronic kidney disease
Biomarker testing trends in metastatic non-small cell lung cancer
Gestational diabetes screening in real world practice
What adolescent sleep disorders reveal about mental health trends