COVID-19 impacted communities disproportionately [1]. Especially in the early days of the pandemic, countless reports of inequitable access to treatments and treatment pathways brought to light existing and new disparities in health outcomes [2]. Addressing health equity is a critical component of Truveta’s vision of saving lives with data.
One of the first steps to addressing disparities is to learn more: For a specific outcome or set of outcomes, who is most impacted? How do differences in access, treatment, or outcomes present? Did the differences persist before and/or throughout the pandemic, or were there different timeframes that exacerbated the disparities?
When looking at a subset of the Truveta Data, we found a higher percentage of Black or African American (henceforth referred to as *Black) individuals were hospitalized with COVID than we would expect based on proportion of Black individuals in the Truveta population – especially early in the pandemic. We also found a larger percentage of hospitalizations for men and older individuals compared to the overall Truveta population.
Methods:
A subset of the de-identified medical records from the Truveta data were used in this study from March 1, 2020 to June 22, 2022. We identified people who were hospitalized with a positive COVID lab test or diagnostic test. We also included people who were hospitalized within 30 days of their initial COVID diagnosis if there was still a positive COVID lab test or diagnostic code related to the inpatient encounter.
We looked at the demographics (age, sex, race, and ethnicity) of people who had been hospitalized across four different time periods in the pandemic:
- Wild: March 1, 2020 – May 31, 2020 (Sample size: ~7,100)
- December 2020: December 1, 2020 – February 28, 2021 (Sample size: ~16,900)
- Delta: June 1, 2021 – August 31, 2021 (Sample size: ~12,300)
- Omicron: December 1, 2021 – February 28, 2022 (Sample size: ~30,000)
We aligned the time periods to COVID spikes across the pandemic. Note that these periods do not indicate that the people in each population had the specific variant. Those data are not included in this analysis.
We also provided a comparison to demographics within the Truveta Data.
Results:
In total, more than 66,000 people who were hospitalized with COVID during these specific time periods were included in this analysis. The population size increased as the pandemic progressed, with the largest population during the Omicron wave at nearly 30,000 patients hospitalized with COVID.
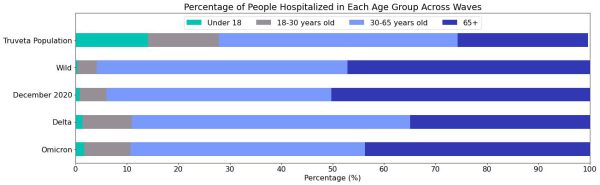
Age:
Across all pandemic periods, we see that older individuals are hospitalized at a higher percentage than the percentage of the population they comprise. As the pandemic has progressed, we see an increase in the percentage of individuals under the age of 30 who are hospitalized with COVID.
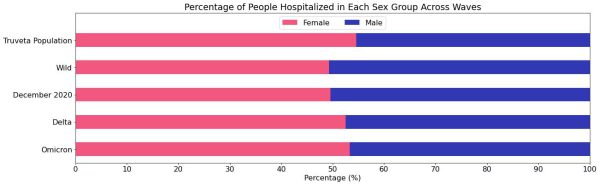
Sex:
Males were hospitalized at a higher rate than expected based on the ratio of females to males in the overall Truveta population (54.6% are female).
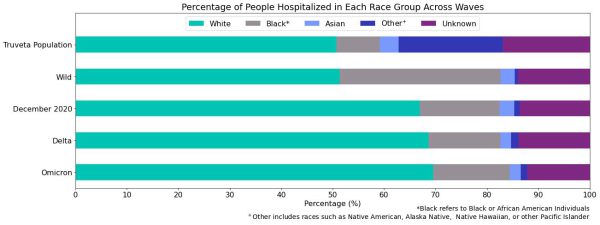
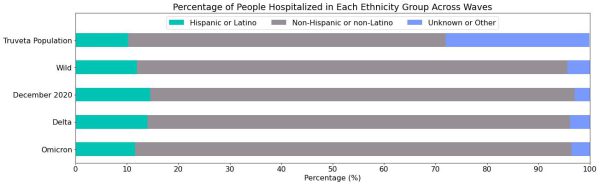
Race and Ethnicity:
When we look across race and ethnicity groups, we see a higher percentage of Black individuals hospitalized with COVID than expected based on the percentage they make up in the Truveta population, especially during the beginning of the pandemic. We also see higher rates of Hispanic or Latino individuals hospitalized, especially during the December 2020 period.
Discussion:
In this blog we show the variation in demographics of people hospitalized with COVID across different periods of the pandemic in a large sample from across the United States. These data show a glimpse into disparities across pandemic waves. The variation we see in racial groups is consistent with previous reports of increased COVID hospitalizations among Black and Hispanic or Latino individuals during the same time [2].
As with all studies, this study is not without limitations. First, patients in this study were included if they had a COVID diagnosis associated with their admission. However, this does not necessarily indicate that patients were hospitalized for COVID; they could have been found to have COVID after being hospitalized for something else. Second, the unknowns in this report either indicate the value was not included in the individual’s electronic health record or that it was excluded from the data to protect an individual’s identity as a part of Truveta’s commitment to privacy [3].
Despite these limitations, the data presented here spark many additional questions for our team: Within this population do we see disparities across social determinants of health (SDOH)? Across the pandemic periods, are there differences in the SDOH features for people who were hospitalized with COVID-19? How did outcomes such as length of stay and medication administration vary across populations? As a research team, we’re excited to continue exploring some of these questions in the future.
* Note: The term “Black” refers to all patients within the Truveta Data who have identified as Black or African American in their electronic medical record.
The analysis in this report laid the groundwork for our published peer-reviewed paper in Frontiers in Public Health: Racial inequality in COVID treatment and in-hospital length of stay in the US over time.
Citations:
[1] Tai, Don Bambino Geno, et al. “The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States.” Clinical Infectious Diseases 72.4 (2021): 703-706.
[2] Acosta AM, Garg S, Pham H, et al. Racial and Ethnic Disparities in Rates of COVID-19–Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death in the United States From March 2020 to February 2021. JAMA Netw Open. 2021;4(10):e2130479. doi:10.1001/jamanetworkopen.2021.30479
[3] Truveta. Our Approach to protecting Patient Privacy. Spring 2022. Truveta’s Approach to Patient Privacy.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data from June 22, 2022.
