UPDATE 1/11/2023: The analysis in this blog has been published as a part of a peer-reviewed paper in Frontiers in Public Health: Racial inequality in COVID treatment and in-hospital length of stay in the US over time.
Many researchers have goals to conduct novel science, uncover new trends, report findings that increase knowledge on a given topic, and push the field forward. To accomplish these goals, there are multiple steps including reviewing prior literature, collecting preliminary data, conducting exploratory analyses, and finally generating a question and hypothesis the researcher has the data to answer. Depending on the outputs of the analysis, the researcher then embarks on the publication process.
At Truveta, we think about this process with one addition: we use our Research Insights to conduct exploratory analyses to inform the question we will study. Insights give us an opportunity to glean knowledge from unadjusted data to see initial results and inform future research. If we find intriguing preliminary results in our exploration, we dig deeper. We continue to dig until we find a place where we think we have a research question worthy of a pre-print and/or peer-reviewed paper. This process allows our team to quickly iterate on projects. We ask questions, interpret results, ask more questions, and ultimately get to a point in which we believe our findings are worthy contributions to the literature.

Truveta Research recently used Truveta Studio to explore potential racial and ethnic disparities in COVID hospitalizations during different time periods throughout the pandemic.
Many research and news outlets have reported on the racial disparities in both those who were infected with COVID-19 and death rates due to COVID [1, 2, 3]. Within our data we were curious if there were disparities in who was hospitalized with COVID across different periods of the pandemic.
Our findings showed that a larger percentage of Black or African American (henceforth referred to as Black) individuals were hospitalized at higher rates than the percentage of the data they make up, especially from March 2020 – May 2020. This led us to a second question: Of the people who were hospitalized with COVID, did the length of stay in the hospital vary by race?
Overall, in our data we found a decreased length of stay by approximately two days from March 2020 – May 2022 for the entire population. However, during March 2020 – May 2020 and December 2020 – February 2021, the length of stay for Black individuals was roughly half a day longer than white individuals. We also found differences by age and sex. When asking both questions, we did not adjust for age or comorbidities that may impact the findings.
This set of exploratory analyses led us to a third analysis with two questions: 1) Was there a difference in who was treated with remdesivir? Remdesivir was the first antiviral drug given emergency use authorization by the US Food and Drug Administration [4, 5]. 2) After adjusting for age, sex, and comorbidities, did we still see differences in length of stay by race, across different periods of the pandemic?
After adjusting for potential confounders, we found Black patients were less likely to receive remdesivir compared to white patients from December 2020 to February 2021. We did not see these trends during the Delta or Omicron periods. We also found increased length of stay occurred for Black patients compared to white patients in all time periods studied besides Omicron, after adjusting for confounders. To learn more about our methods and the specifics of the trends, check out the full peer-reviewed research published in Frontiers in Public Health: Racial inequality in COVID treatment and in-hospital length of stay in the US over time.
Methods
We used a subset of Truveta Data from March 1, 2020 to February 28, 2022 in this study. We identified people who were hospitalized with a positive COVID lab test or diagnostic test.
We identified four different time periods in the pandemic:
- Wild: March 1, 2020 – May 31, 2020
- Dec 2020: December 1, 2020 – February 28, 2021
- Delta: June 1, 2021 – August 31, 2021
- Omicron: December 1, 2021 – February 28, 2022
We aligned the time periods to COVID spikes across the pandemic. It is important to note that these periods do not indicate that the people in each population had the specific variant. Those data are not included in this analysis.
Remdesivir was not studied during the Wild period because it received FDA Emergency Use Authorization (EAU) on May 1, 2020, over halfway through the study period [4, 6].
After adjusting for demographic factors (i.e., age, sex) and comorbidities (i.e., diabetes, hypertension, chronic kidney disease, liver disease, immunocompromised state, and cancer), we looked at the difference by race in two outcomes: 1) receipt of remdesivir as a treatment, and 2) length of stay.
Results
The population hospitalized with COVID during the four time periods resulted in approximately 60,000 patients.
Remdesivir treatment
We found that Black individuals were treated with remdesivir at a significantly lower rate (12%) than white individuals during December 2020, after adjustment for demographic and comorbidity factors. Statistically significant trends were not observed during either of the other time periods studied (Delta and Omicron). The figure below shows the results of the model.
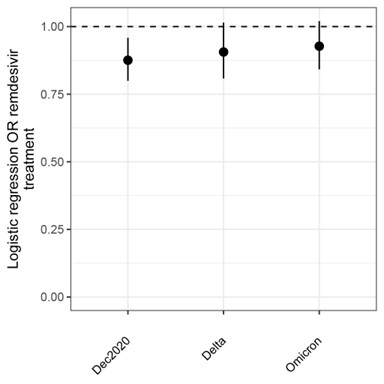
Remdesivir treatment for Black or African American patients compared to white patients hospitalized with COVID during different periods of the pandemic. Values overlapping 1 indicate no difference between groups.
Length of stay
After adjustment for demographic factors and comorbidities, we found Black individuals had a significantly longer length of stay than white individuals at 5%, 16%, and 18% for the Wild, December 2020, and Delta periods. There were no significant differences for Omicron. The figure below shows the results of the model. Values equal to one indicate similar lengths of stay between the two race groups. Values over one indicate a longer length of stay for Black individuals compared with white individuals, while values under one indicate a shorter length of stay for Black individuals compared to white individuals. The length of the bars indicates the confidence in the measurement.
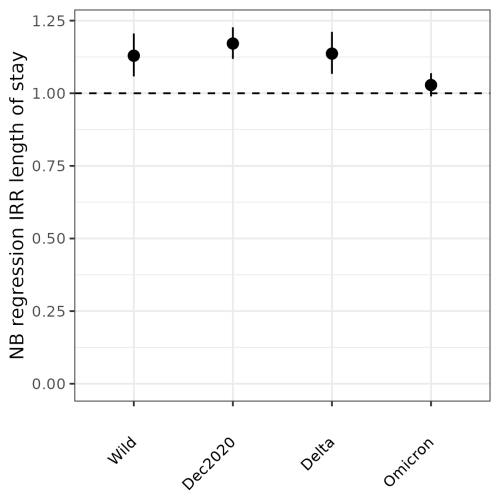
Length of stay for Black or African American patients compared to white patients hospitalized with COVID during different periods of the pandemic. Values overlapping 1 indicate no difference between groups.
Discussion
Using Truveta Data, we can quickly iterate on questions and conduct exploratory analyses that lead us to interesting research questions. We believe this method of exploring data and iterating on our research questions allows us to reach new insights quickly.
Inequalities have existed for decades in healthcare access, timeliness of treatment delivery, and treatment outcomes. Collectively as a society, our ongoing accumulation of knowledge on COVID outcomes, epidemiology, and treatments allows us to better situate disparities across racial groups. Here we find that early in the pandemic, there were broad differences in length of stay and remdesivir treatment between Black patients and white patients. Hearteningly, our sample of over 60,000 COVID-hospitalized patients shows this gap may be closing and approaching parity between the two groups. Policymakers should prioritize continuing to understand where disparities exist and achieving equity in access to healthcare and quality of care.
To learn more about our methods and further discussion of our results, check out the peer-reviewed research in Frontiers in Public Health: Racial inequality in COVID treatment and in-hospital length of stay in the US over time.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data pulled June 22, 2022.
Citations
[1] Khanijahani, Ahmad, et al. “A systematic review of racial/ethnic and socioeconomic disparities in COVID-19.” International journal for equity in health 20.1 (2021): 1-30.
[2] Zelner, Jon, et al. “Racial disparities in coronavirus disease 2019 (COVID-19) mortality are driven by unequal infection risks.” Clinical Infectious Diseases 72.5 (2021): e88-e95.
[3] Mackey, Katherine, et al. “Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: a systematic review.” Annals of internal medicine 174.3 (2021): 362-373.
[4] Eastman, Richard T., et al. “Remdesivir: a review of its discovery and development leading to emergency use authorization for treatment of COVID-19.” ACS central Science 6.5 (2020): 672-683.
[5] Beigel, John H., et al. “Remdesivir for the treatment of Covid-19.” New England Journal of Medicine 383.19 (2020): 1813-1826.
[6] US Food & Drug Administration. “Coronavirus (COVID-19) Update: FDA Issues Emergency Use Authorization for Potential COVID-19 Treatment.” FDA NEWS RELEASE, 01 May 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment.
About Truveta
Truveta is a collective of US health systems with a shared vision of saving lives with data. Truveta offers innovative solutions to enable researchers to find cures faster, empower every clinician to be an expert, and help families make the most informed decisions about their care. To learn more, follow us on LinkedIn and Twitter, and sign up for our newsletter.
