Among women with preeclampsia, new Truveta Research findings show that Black women are two times more likely to experience heart failure than white women.
Maternal health outcomes in the US are worse than in many other high-income countries such as England, France, Korea, Australia, and the Netherlands (Gunja et al., 2022). Preeclampsia is a potentially fatal maternal health condition which occurs in one out of every 25 pregnancies in the United States (Centers for Disease Control and Prevention, 2022b). Preeclampsia is marked by high blood pressure after 20 weeks (5 months) of pregnancy or soon after giving birth. The high blood pressure can only be reduced by giving birth.
This high blood pressure has been linked to heart failure following delivery (Williams et al., 2021); one in every 112 pregnancies leads to heart failure, requiring hospitalization of the mother (Honigberg, 2021). Heart failure occurs when your heart muscle weakens, causing the heart muscle to not pump oxygenated blood to the rest of the body at the rate it should. As a result, other organs throughout the body struggle to function normally. Heart failure in women following delivery is one of the leading causes of death of women following delivery in the United States (Mogos et al., 2018).
Nearly every negative maternal health outcome in the United States affects Black, American Indian, Alaska Native, Native Hawaiian, Pacific Islander, and Hispanic women more than white and non-Hispanic women. In fact, the rates for Black women are so different than the rest of the population that the Centers for Disease Control and Prevention track them separately, in addition to including them in the main population (Centers for Disease Control and Prevention, 2022a; Gunja et al., 2022; US Preventive Services Task Force et al., 2017). Examples include maternal mortality; Black women are three times more likely to die from pregnancy-related causes than white women (Centers for Disease Control and Prevention, 2022a; Petersen et al., 2019) and the rate of unnecessary cesarean delivery. Black women are 21% more likely and Hispanic women are 26% more likely to have a cesarean surgery at first delivery than white or non-Hispanic women, respectively (Debbink et al., 2022). This contributes to an excess of maternal morbidity (including need for hysterectomy) for both populations (15.8% for Black women and 16.5% for Hispanic women) compared to white and non-Hispanic women (Debbink et al., 2022).
Although rare, the impacts of heart failure at and following delivery are important for all women, babies, and families. We wanted to replicate a previous study (Williams et al., 2021) with the Truveta data and understand if we saw racial and ethnic disparities in the rate of women who both developed preeclampsia and subsequent heart failure following delivery.
METHODS
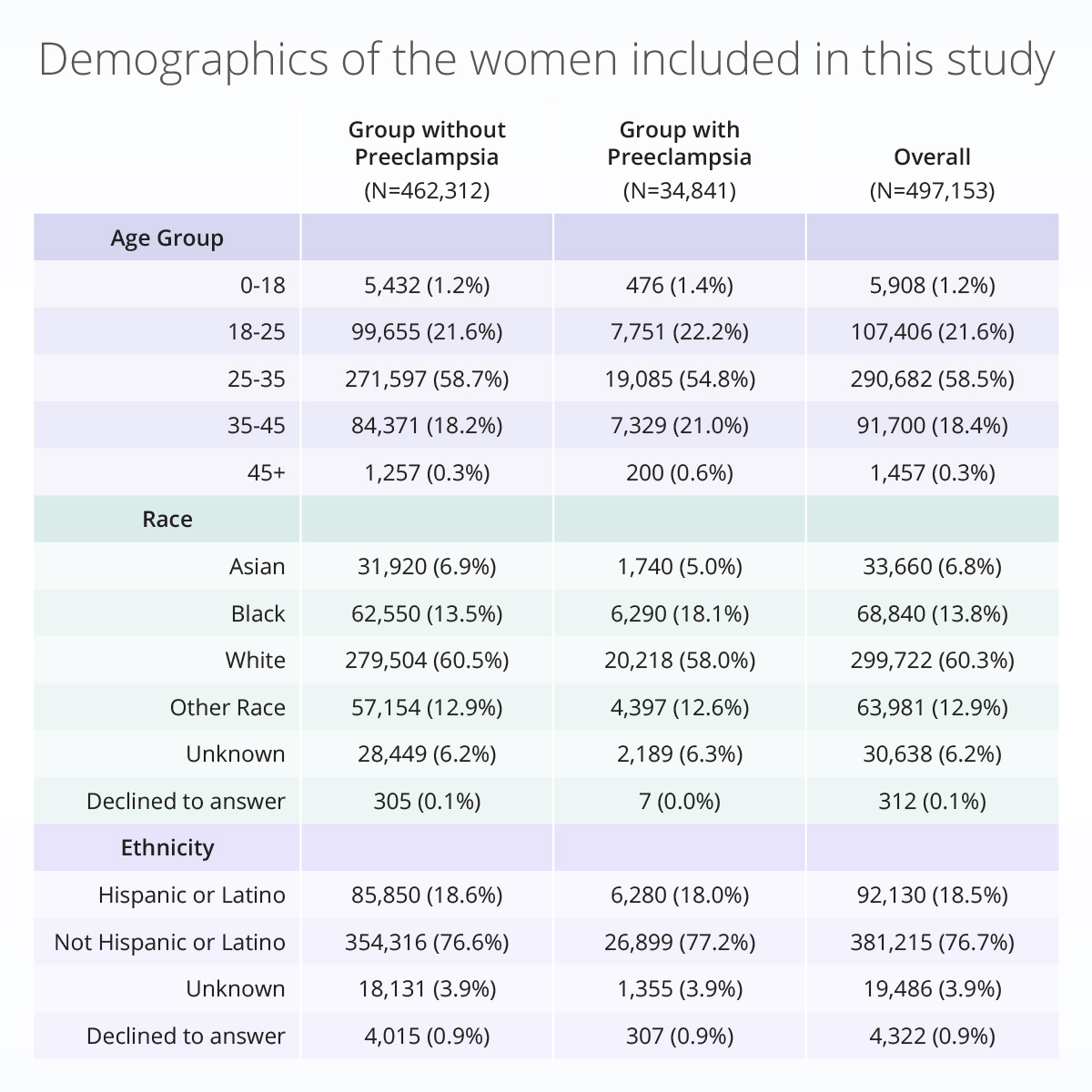
In a subset of Truveta data, we identified the first delivery within the data that did not have a prior history of ischemic heart disease, chronic kidney disease, cardiomyopathy, myocardial infarction, or pulmonary embolism. We excluded people with unknown or male sex. Nearly 500,000 women met our inclusion criteria. Table 1 shows the distribution of women’s age, race, and ethnicity in this data set.
We defined delivery, preeclampsia, and heart failure (including congestive heart failure, heart failure with preserved ejection fracture, and heart failure with reduced ejection fraction) using the ICD-10-CM and SNOMED CT codes. A patient was considered to have preeclampsia if either preeclampsia or eclampsia appeared in their record during the current pregnancy, but no later than the day of delivery. This will henceforth be referred to as preeclampsia. Patients were considered to have heart failure if it occurred on the day of delivery or within 90 days of delivery. Patients without any records after their delivery were excluded from analysis unless they experienced heart failure on their day of delivery.
To see if the chance of developing heart failure was different based on whether a patient had preeclampsia, we calculated the odds ratio. This calculation compares the chance of something happening to it not happening. For example, one could use the odds ratio to determine the chance of winning the lottery if they play daily to the chance of winning the lottery if they play once a year. In this case, we wanted to compare the chance of having heart failure if a woman had preeclampsia to the chance of having heart failure if a woman did not have preeclampsia. We took this a step further and investigated whether there were differences (there were disparities) by race or ethnicity. It is important to note, due to size of the population we only compared differences between Black, Asian, and white mothers. The other race groups were bucketed into one ‘other race’ category.
RESULTS
Of the 497,153 deliveries that met our inclusion criteria, 34,841 had preeclampsia. Most deliveries were for women between the ages of 25 years and 35 years. The majority of deliveries were for women that were white (60.3%), followed by women that were Black (13.8%), and women with other race categories not otherwise captured in these data (11.6%). 18.5% of women were Hispanic or Latino.
If you were to roll a six-sided die, you have a 1 out of 6 chance to roll any of the numbers on the die. The chance is equal no matter the side.
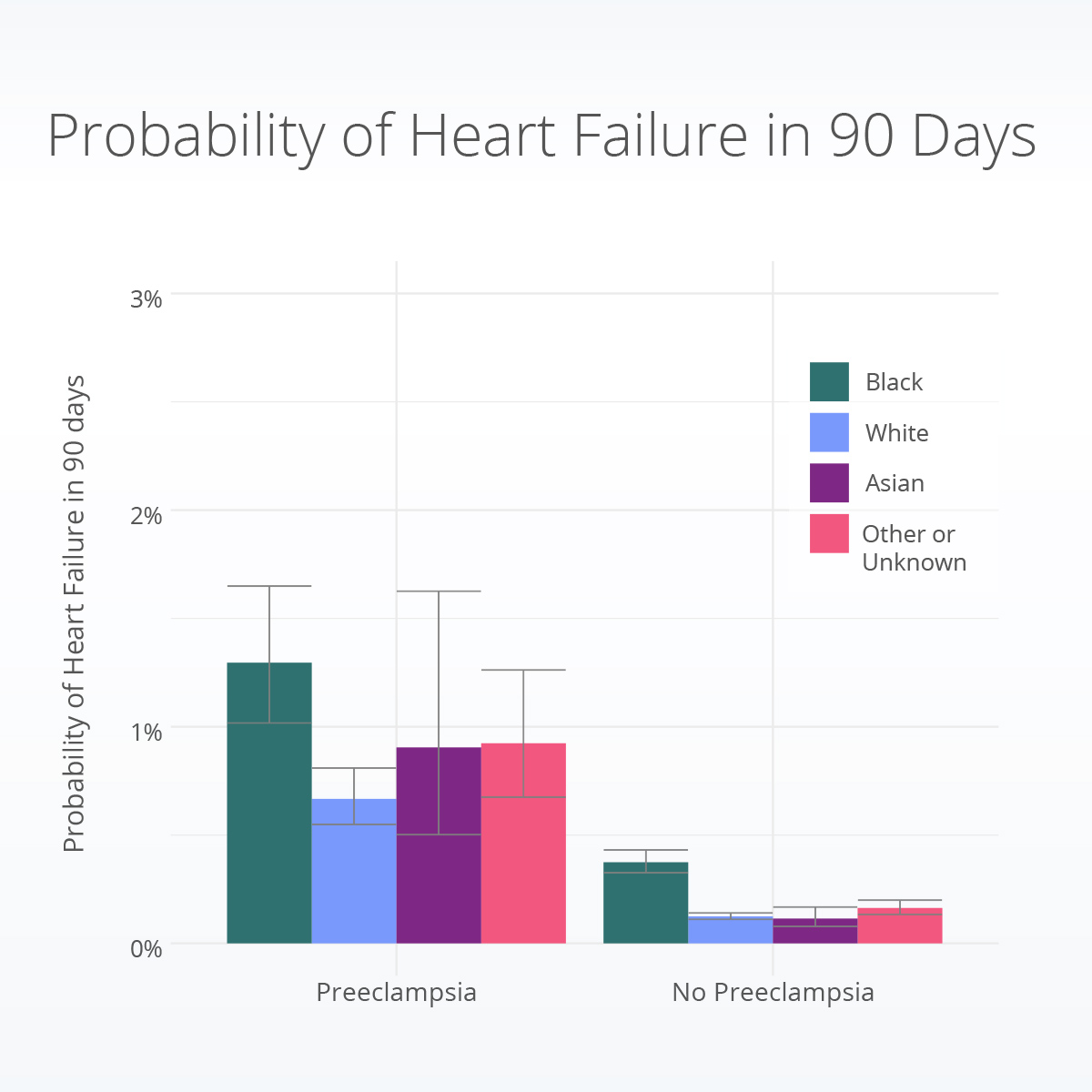
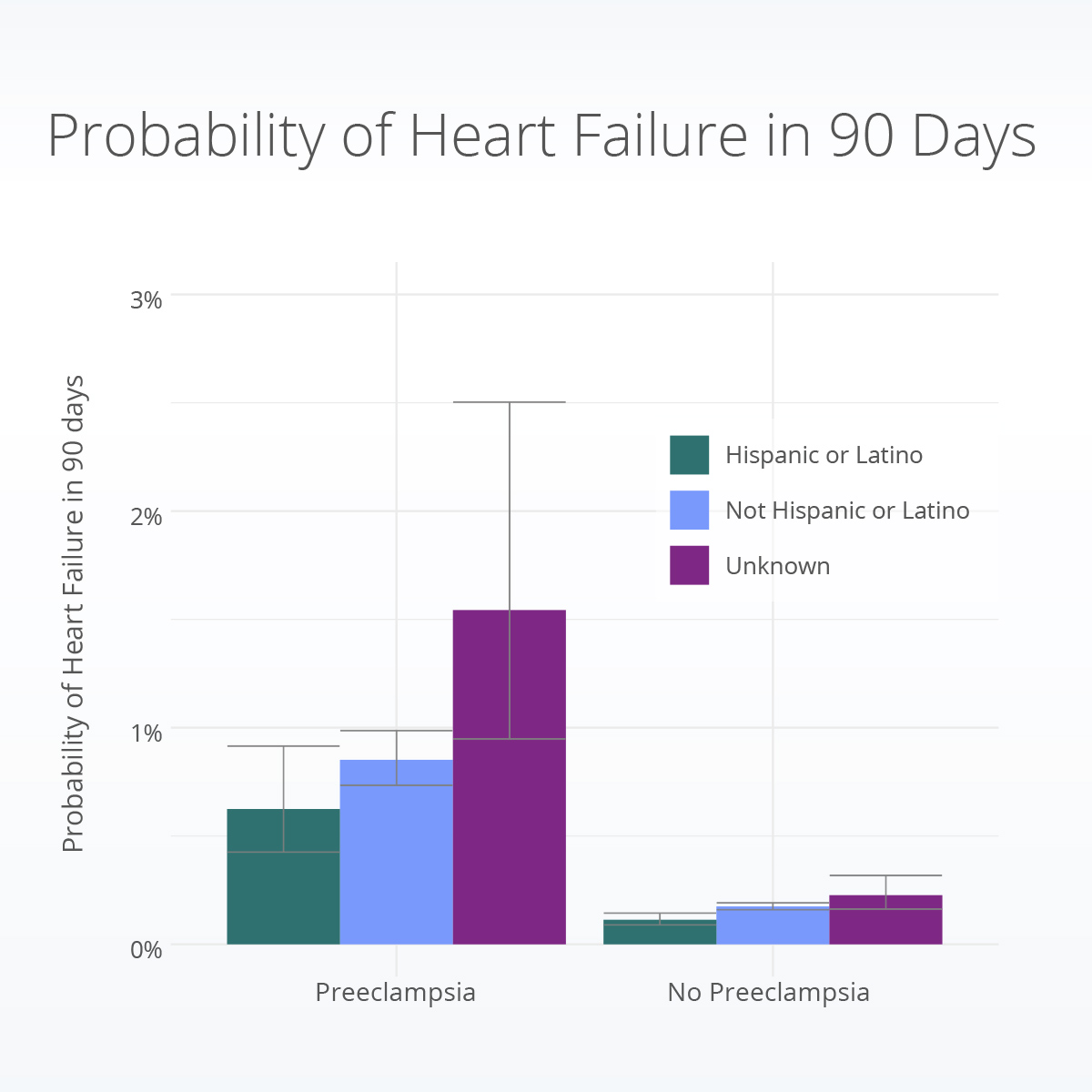
Is heart failure more likely if a woman experiences preeclampsia? Our results show the chance of having heart failure within 90 days of delivery is greater for women who experienced preeclampsia during their pregnancy. We also found this to be true within each race group; white women with preeclampsia were 5.3 times, Black women were 3.5 times, and Asian women were 8.0 times more likely to have heart failure post-delivery than their counterparts without preeclampsia. Similarly, Hispanic or Latino women were 5.5 times, non-Hispanic or non-Latino women were 4.9 times, and women of unknown or other Hispanic or Latino ethnicity were 6.9 times more likely to experience heart failure post-delivery than their counterparts without preeclampsia.
Are there racial and ethnic disparities in heart failure following delivery for women with preeclampsia? When we compare results for Black and white women, Black women with preeclampsia are 2.0 times as likely to have heart failure compared to white women with preeclampsia. Black women with preeclampsia are 1.4 times more likely to have heart failure than Asian women with preeclampsia. We did not identify significant differences in likelihood of heart failure onset after preeclampsia between women of Hispanic or Latino ethnicity and those not of Hispanic or Latino ethnicity.
Discussion/Conclusion
The results of this study are important for many reasons. First, in this study we replicated previous work showing the connection between preeclampsia during pregnancy and increased risk for heart failure following delivery. Further, we build upon the current literature to show disparities in who is most at risk for heart failure following delivery. More research is needed to learn the specifics of why preeclampsia during pregnancy causes increased risk for heart failure and what physicians and obstetricians can do to prevent it. This includes the need to learn what factors about women, their care, their families, or their communities we can change which will have the biggest impacting in reducing the chance for heart failure, preeclampsia, or the combination.
These results make us curious about other outcomes following pregnancy and the factors that influence these outcomes, specifically those related to disability, social determinants of health, teen pregnancy, and advanced maternal age pregnancy. We plan to look deeper into the different types of heart failure and the impact of chronic high blood pressure prior to pregnancy on these outcomes.
One limitation of this analysis is that we only included women who reached delivery; if a woman had an abortion or miscarriage they would not be included in this analysis. Further, if a woman delivered inside a Truveta health system, but receives usual care at another heath system, these data would miss subsequent encounters. We tried to account for this by excluding women who did not have any encounters following the delivery encounter. Additionally, we only looked at heart failure as an overall concept; we could also include details of specific types of heart failure such as HFpEF in future versions.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data pulled January 25, 2023.
CITATIONS
Gunja, M. Z., Gumas, E. D., & Williams II, R. D. (2022). The U.S. Maternal Mortality Crisis Continues to Worsen: An International Comparison. https://doi.org/10.26099/8VEM-FC65
Centers for Disease Control and Prevention. (2022, December 13). High Blood Pressure During Pregnancy. https://www.cdc.gov/bloodpressure/pregnancy.htm
Williams, D., Stout, M. J., Rosenbloom, J. I., Olsen, M. A., Joynt Maddox, K. E., Deych, E., Davila-Roman, V. G., & Lindley, K. J. (2021). Preeclampsia Predicts Risk of Hospitalization for Heart Failure With Preserved Ejection Fraction. Journal of the American College of Cardiology, 78(23), 2281–2290. https://doi.org/10.1016/j.jacc.2021.09.1360
Honigberg, M. C. (2021). Understanding Heart Failure in Women With Preeclampsia. Journal of the American College of Cardiology, 78(23), 2291–2293. https://doi.org/10.1016/j.jacc.2021.09.1361
Mogos, M. F., Piano, M. R., McFarlin, B. L., Salemi, J. L., Liese, K. L., & Briller, J. E. (2018). Heart Failure in Pregnant Women: A Concern Across the Pregnancy Continuum. Circulation: Heart Failure, 11(1), e004005. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004005
Centers for Disease Control and Prevention. (2022, April 6). Working Together to Reduce Black Maternal Mortality. https://www.cdc.gov/healthequity/features/maternal-mortality/index.html
Centers for Disease Control and Prevention. (2022, April 6). Working Together to Reduce Black Maternal Mortality. https://www.cdc.gov/healthequity/features/maternal-mortality/index.html
US Preventive Services Task Force, Bibbins-Domingo, K., Grossman, D. C., Curry, S. J., Barry, M. J., Davidson, K. W., Doubeni, C. A., Epling, J. W., Kemper, A. R., Krist, A. H., Kurth, A. E., Landefeld, C. S., Mangione, C. M., Phillips, W. R., Phipps, M. G., Silverstein, M., Simon, M. A., & Tseng, C.-W. (2017). Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement. JAMA, 317(16), 1661. https://doi.org/10.1001/jama.2017.3439
Petersen, E. E., Davis, N. L., Goodman, D., Cox, S., Syverson, C., Seed, K., Shapiro-Mendoza, C., Callaghan, W. M., & Barfield, W. (2019). Racial/Ethnic Disparities in Pregnancy-Related Deaths—United States, 2007–2016. MMWR. Morbidity and Mortality Weekly Report, 68(35), 762–765. https://doi.org/10.15585/mmwr.mm6835a3
Debbink, M. P., Ugwu, L. G., Grobman, W. A., Reddy, U. M., Tita, A. T. N., El-Sayed, Y. Y., Wapner, R. J., Rouse, D. J., Saade, G. R., Thorp, J. M., Chauhan, S. P., Costantine, M. M., Chien, E. K., Casey, B. M., Srinivas, S. K., Swamy, G. K., Simhan, H. N., & for the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network. (2022). Racial and Ethnic Inequities in Cesarean Birth and Maternal Morbidity in a Low-Risk, Nulliparous Cohort. Obstetrics & Gynecology, 139(1), 73–82. https://doi.org/10.1097/AOG.0000000000004620
About Truveta
Truveta is a collective of US health systems with a shared vision of saving lives with data. Truveta offers innovative solutions to enable researchers to find cures faster, empower every clinician to be an expert, and help families make the most informed decisions about their care. To learn more, follow us on LinkedIn, sign up for our newsletter, and contact us below for a demo.