Authors: Brianna M. Goodwin Cartwright ⊕Truveta, Inc, Bellevue, WA, Patricia J. Rodriguez, PhD MPH ⊕Truveta, Inc, Bellevue, WA, Samuel Gratzl PhD ⊕Truveta, Inc, Bellevue, WA, Charlotte Baker DrPH MPH CPH ⊕Truveta, Inc, Bellevue, WA, Christopher M. Worsham, MD MPH ⊕Department of Health Care Policy, Harvard Medical School, Boston, MA
Department of Medicine, Massachusetts General Hospital, Boston, MA
Division of Pulmonary and Critical Care Medicine, Massachusetts General Hospital, Boston, MA, Anupam B. Jena, MD PhD ⊕Department of Health Care Policy, Harvard Medical School, Boston, MA
Department of Medicine, Massachusetts General Hospital, Boston, MA
National Bureau of Economic Research, Cambridge, MA, Nicholas Stucky, MD PhD ⊕Truveta, Inc, Bellevue, WA
- With the growing popularity of GLP-1 RAs, concerns have been raised that the expanded use may occur amongst patients with less clinical need.
- For a population of people with type 2 diabetes and first-time GLP-1 RA prescriptions, we found decreases in baseline A1C and BMI values (prior to GLP-1 RA initiation) between January 2020 and November 2023. A1C values were still higher than the clinical value used to diagnose diabetes.
- We found higher A1C and BMI values for people with lower incomes in January 2020. A1C values decreased over the time period for all income groups, while trends in BMI values varied by income.
This blog is an extension of our poster presented at ISPOR 2024, titled Baseline A1C and BMI trends for people with type 2 diabetes receiving first-time GLP-1 RA prescriptions.
The popularity of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) has increased in recent years (Rodriguez et al., 2023). This class of drugs has shown to be effective in lowering blood sugar to better control type 2 diabetes (T2D) and induce weight loss (Dahl et al., 2022; Davies et al., 2021; Garvey et al., 2022, 2023; Goldenberg & Steen, 2019; Jastreboff et al., 2022). This has fueled attention for these drugs in mainstream media, TikTok promotion, and endorsement by celebrities and celebrity doctors, further raising awareness of this drug class (Belluz, 2023; Bienasz, 2023; Nelson, 2023; Smith, 2023).
More recently, concerns have been raised that the rapid expanded use may be to patients with less clinical need. This, in turn, could raise costs for all patients. In this study, we explored whether A1C and BMI values – measures of clinical need – have decreased over time for people with T2D newly prescribed a GLP-1 RA medication. We looked at effects overall and when stratified by income group.
You can also view this study in Truveta Studio.
Methods
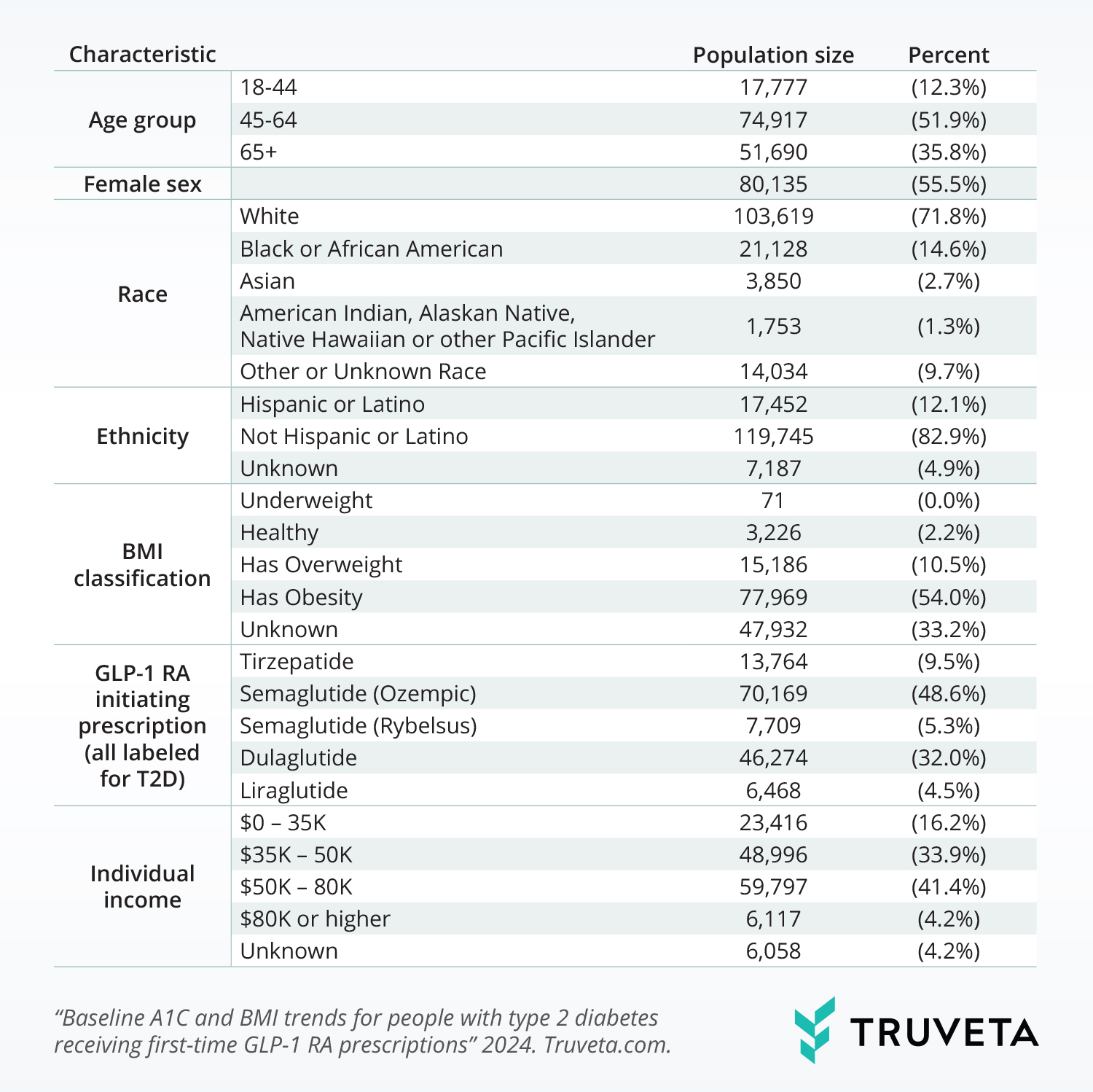
Using a subset of Truveta Data, we identified people with a T2D diagnosis, who were prescribed a first-time T2D-labeled GLP-1 RA (dulaglutide, semaglutide – oral, semaglutide – injectable, tirzepatide, and liraglutide) between January 2020 and November 2023. Patients were also required to be adults (age 18 or over) and have a dispense of any medication at any time. They were excluded if they had a prior diagnosis of type 1 or gestational diabetes or received a drug during the month it was approved by the FDA or prior month.
The most recent A1C and BMI values, within the year prior, to the new GLP-1 RA prescription were determined and used in the analysis (referred to as baseline values). Values outside acceptable range were excluded (A1C: 0-20%, BMI: 0-100). Separate linear mixed effects models were used to test for changes in baseline A1C and BMI over time, using a random effect to account for variation in level by drug. We additionally created models with interaction terms between individual income and time to test for changes in income across time. A likelihood ratio test was used to test whether models differed with the inclusion of income by time interactions.
Results
We included 144,384 patients with T2D and a first-time GLP-1 RA prescription during the study period. The population was primarily between the ages of 45-64 (51.9%), female (55.5%), white (71.8%), and not Hispanic or Latino (82.9%). A1C values were available for 71.8% of the population, and patients had an average baseline value of 8.1 ± 1.8%. BMI values were available for 66.8% of the population, with an average baseline value of 37.0 ± 8.3.
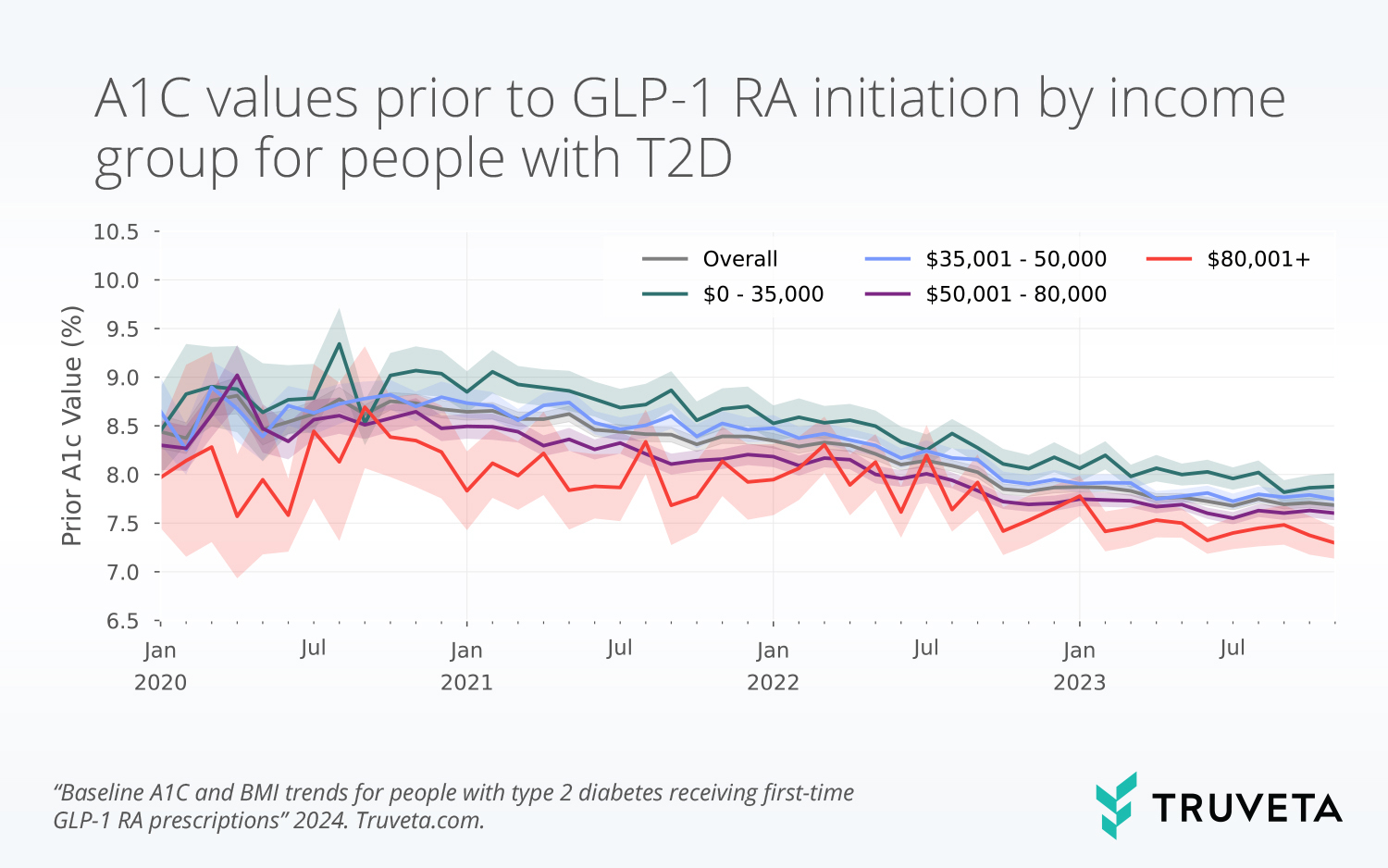
A1C models
Without including the effects of income, at baseline (January 2020), the mean A1C value was 8.7% (p<0.001) and decreased significantly over time (-0.02% per month, p<0.001). This indicates that, on average, A1C values decreased by 0.02% each month.
The model – which included income and income by time interactions – had the highest baseline A1C value for people with the lowest incomes ($0-35K: 9.0%, p<0.001) and decreased steadily by income level ($35–50K: 8.8%, $50–80K: 8.5%, $80K+: 8.2%, p<0.001). A1C also decreased significantly over time, with the largest decrease in the group with incomes $0–35K (-0.025%, p<0.001), and smaller decreases for higher income groups ($35–50K: -0.024%, p=0.3, $50–80K: -0.02%, p<0.001, $80K or higher: -0.016%, p<0.001) compared to the $0 – 35K group.
The likelihood ratio test confirmed models with and without the inclusion of income were significantly different.
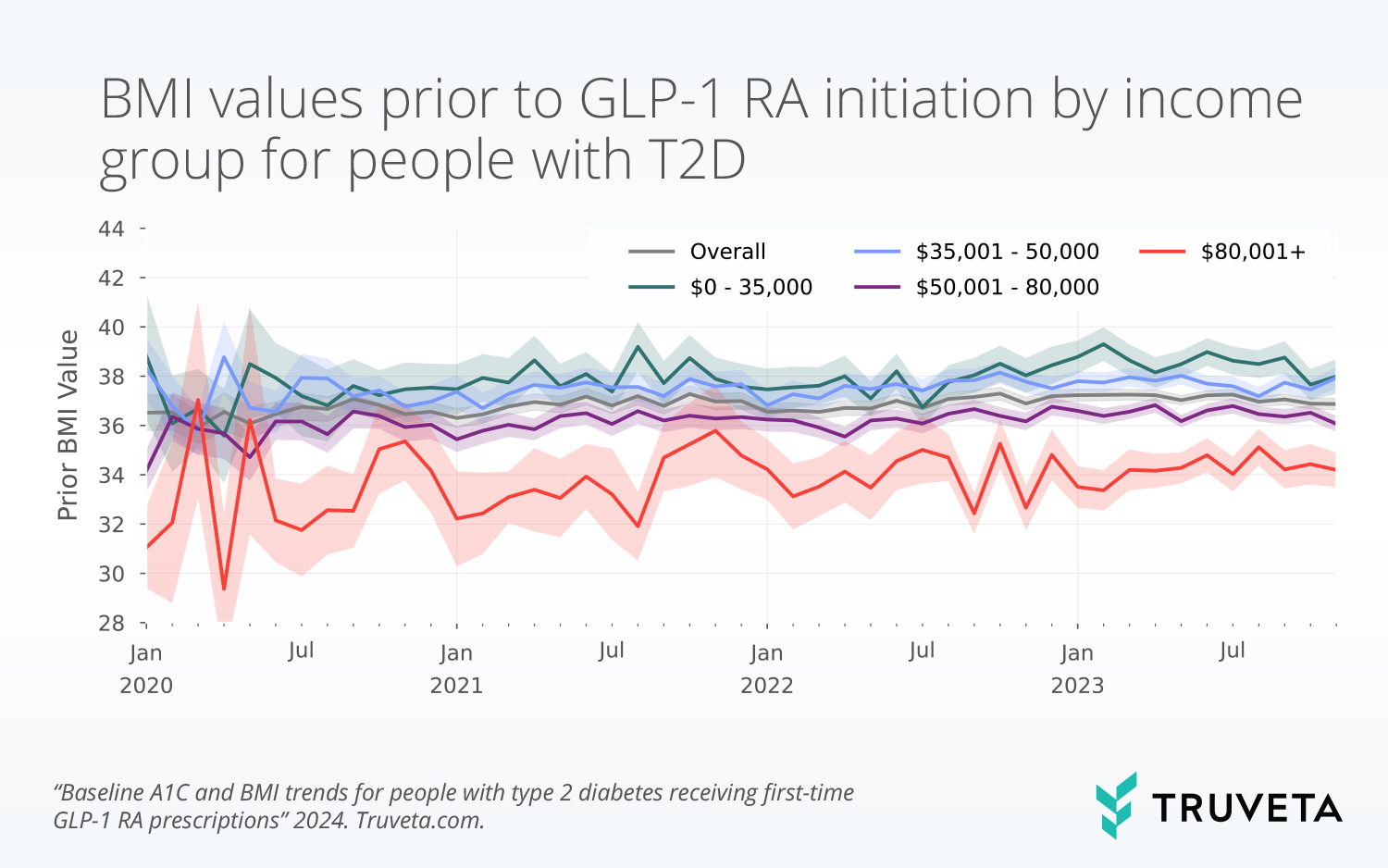
BMI models
Without income, the mean baseline BMI was 37.4 (p<0.001) and decreased significantly over time (-0.01 per month, p<0.001).
With the inclusion of income and income by time interactions, the mean BMI at baseline was highest for those with the lowest incomes ($0-35K: 38.1, p<0.001). The baseline BMI value decreased by income level ($35–50K: 38.0, p = 0.6; $50–80K: 36.7, p<0.011; $80K+: 34.2, p<0.001). There was no significant change over time for those with incomes $0-35K, and a small but significant decrease for those with incomes between $35–50K (-0.011, p = 0.009) and $50–80K (-0.012, p = 0.004) compared to the $0–35K group.
Similar to the A1C results, the likelihood ratio test confirmed models with and without the inclusion of income were significantly different.
Discussion
In this study, we aimed to understand if people with T2D, who were newly prescribed GLP-1 RAs labeled for T2D, were initiating treatment at markers indicative of lower disease severity. Since 2020, we found lower baseline A1C and BMI values for this population over time, indicating that people are initiating GLP-1 RA at healthier levels. However, although the mean baseline A1C over time has decreased for people with T2D, at the end of the study period, the A1C value was still over 6.5% (the percent at which diabetes is diagnosed) (Centers for Disease Control and Prevention, 2022). Although more recent GLP-1 RA initiators are healthier, they still have A1C values consistent with diabetes.
Both A1C and BMI models that included income showed that individuals in the lowest income groups had the highest A1C and BMI values. This finding is consistent with previous literature that individuals with lower incomes have higher disease burden (Beckles & Chou, 2016; Chen et al., 2023). Further, higher baseline BMI and A1C may suggest that lower income individuals wait longer to add second line therapies, like GLP-1 RAs, potentially due to the high cost relative to first line therapies (such as metformin). Decreases over time varied by income groups, which may indicate different treatment patterns by income groups since 2020. The differences seen by income groups may be influenced by both the increased use of GLP-1 RAs during the study period (Rodriguez et al., 2023) and the change in clinical guidelines during the period (“Summary of Revisions,” 2020).
There are a few limitations with this analysis. First, we did not look at effectiveness of these drugs – the values reported here were found prior to initiation of the prescriptions, and thus, cannot be used to infer drug effectiveness over time. Second, an initial prescription was used as intent to treat however, we did not require people to have a subsequent medication dispense. Therefore, people may not have received GLP-1 RA treatment or may have initiated treatment on a different GLP-1 RA than the one they were prescribed.
These findings are consistent with data accessed on January 2, 2024.
You can also view this study in Truveta Studio.
Citations
Beckles, G. L., & Chou, C.-F. (2016). Disparities in the Prevalence of Diagnosed Diabetes—United States, 1999–2002 and 2011–2014. MMWR. Morbidity and Mortality Weekly Report, 65(45), 1265–1269. https://doi.org/10.15585/mmwr.mm6545a4
Belluz, J. (2023, February 7). Obesity in the age of Ozempic. Vox. https://www.vox.com/science-and-health/23584679/ozempic-wegovy-semaglutide-weight-loss-obesity
Bienasz, G. (2023, March 3). Doctors Are Promoting Weight Loss Drugs like Ozempic and Wegovy on TikTok. Entrepreneur. https://www.entrepreneur.com/business-news/tiktok-docs-boosting-views-and-profits-with-weight-loss/446905
Centers for Disease Control and Prevention. (2022, September 30). All About Your A1C. https://www.cdc.gov/diabetes/managing/managing-blood-sugar/a1c.html
Chen, Y., Zhou, X., Bullard, K. M., Zhang, P., Imperatore, G., & Rolka, D. B. (2023). Income-related inequalities in diagnosed diabetes prevalence among US adults, 2001−2018. PLOS ONE, 18(4), e0283450. https://doi.org/10.1371/journal.pone.0283450
Dahl, D., Onishi, Y., Norwood, P., Huh, R., Bray, R., Patel, H., & Rodríguez, Á. (2022). Effect of Subcutaneous Tirzepatide vs Placebo Added to Titrated Insulin Glargine on Glycemic Control in Patients With Type 2 Diabetes: The SURPASS-5 Randomized Clinical Trial. JAMA, 327(6), 534. https://doi.org/10.1001/jama.2022.0078
Davies, M., Færch, L., Jeppesen, O. K., Pakseresht, A., Pedersen, S. D., Perreault, L., Rosenstock, J., Shimomura, I., Viljoen, A., Wadden, T. A., & Lingvay, I. (2021). Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): A randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. The Lancet, 397(10278), 971–984. https://doi.org/10.1016/S0140-6736(21)00213-0
Garvey, W. T., Batterham, R. L., Bhatta, M., Buscemi, S., Christensen, L. N., Frias, J. P., Jódar, E., Kandler, K., Rigas, G., Wadden, T. A., Wharton, S., & the STEP 5 Study Group. (2022). Two-year effects of semaglutide in adults with overweight or obesity: The STEP 5 trial. Nature Medicine, 28(10), 2083–2091. https://doi.org/10.1038/s41591-022-02026-4
Garvey, W. T., Frias, J. P., Jastreboff, A. M., Le Roux, C. W., Sattar, N., Aizenberg, D., Mao, H., Zhang, S., Ahmad, N. N., Bunck, M. C., Benabbad, I., Zhang, X. M., Abalos, F. H., Manghi, F. C. P., Zaidman, C. J., Vico, M. L., Aizenberg, D., Costanzo, P. R., Serra, L. P., … Jones, T. (2023). Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): A double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. The Lancet, 402(10402), 613–626. https://doi.org/10.1016/S0140-6736(23)01200-X
Goldenberg, R. M., & Steen, O. (2019). Semaglutide: Review and Place in Therapy for Adults With Type 2 Diabetes. Canadian Journal of Diabetes, 43(2), 136–145. https://doi.org/10.1016/j.jcjd.2018.05.008
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., Wharton, S., Connery, L., Alves, B., Kiyosue, A., Zhang, S., Liu, B., Bunck, M. C., & Stefanski, A. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine, 387(3), 205–216. https://doi.org/10.1056/NEJMoa2206038
Nelson, E. L. (2023, April 7). 8 Celebrities Who’ve Admitted to Using Ozempic. BestLife. https://bestlifeonline.com/celebrities-who-took-ozempic/
Rodriguez, P. J., Gratzl, S., Goodwin Cartwright, B. M., Brar, R., Gluckman, T. J., & Stucky, N. L. (2023). First-Time Prescribing of GLP-1 Receptor Agonists from 2018-2023: A Descriptive Analysis. https://doi.org/10.1101/2023.08.22.23294277
Smith, R. (2023, January 18). Celebrities Who Have Spoken Out About Hollywood Weight Loss Drug Ozempic. Newsweek. https://www.newsweek.com/celebrities-hollywood-weight-loss-diabetes-drug-ozempic-1774677
Summary of Revisions: Standards of Medical Care in Diabetes—2020. (2020). Diabetes Care, 43(Supplement_1), S4–S6. https://doi.org/10.2337/dc20-Srev