- Adalimumab (Humira) and etanercept (Enbrel) are high-cost specialty medications used to treat a variety of autoimmune diseases. Medication adherence is often influenced by social drivers of health, so we aimed to measure adherence using the proportion of days covered and estimate the effects of race, ethnicity, age, sex, income, marital status, education, and address stability.
- We found significantly higher rates of medication adherence amongst those taking adalimumab for males and people who were married. We did not see any significant associations for the population taking etanercept.
Medication adherence is a critical aspect of managing many conditions, including autoimmune diseases; poor adherence is also estimated to cost the US healthcare systems nearly $300 million annually (American Heart Association, 2023). TNF blockers, such as adalimumab (Humira) and etanercept (Enbrel), are commonly prescribed treatments for a variety of autoimmune diseases, such as Crohn’s disease and rheumatoid arthritis. Ensuring consistent and timely administration of these biologic therapies is essential to reduce inflammation and control disease progression. However, their effectiveness hinges on adhering to the prescribed dosing schedules, typically administered through injections. In general, patients who diligently adhere to these schedules are more likely to experience symptom relief, halt disease progression, and improve their overall quality of life. We have previously reported about medication adherence related to people with type 2 diabetes; however, the specialty drugs studied here are often much more expensive than SGLT2i drugs or metformin.
Without insurance, both adalimumab and etanercept can cost thousands of dollars for a single dose, although with insurance the prices can be more affordable (Drugs.com, 2023; Drugs.com & Anderson, 2023). Increased drug costs are associated with decreased medication adherence rates (Phillion, 2022). Further, medication non-adherence has been positively correlated with many social drivers of health (SDOH); for example, existing financial strain can lead to challenges high-cost drugs, low patient literacy levels can make it challenging to understand all medication instructions without additional help (Jimmy & Jose, 2011), and lack of access to healthcare and decreased social support can increase the challenges people patients face in accessing their medications (DiMatteo, 2004; Osborn et al., 2017).
We set out to understand how first-year medication adherence for patients initiating adalimumab or etanercept varied by social drivers of health (SDOH).
Methods
Looking at a subset of Truveta Data, we identified people who initiated treatment for adalimumab or etanercept between January 1, 2016 and August 31, 2023. Treatment initiation was defined as a first-time prescription and a dispensed medication within 60 days.
People were excluded if they were less than 18 years old at the time of their first prescription, received a prescription or dispense for another drug within the TNF blocker class (infliximab (Remicade), golimumab (Simponi), or certolizumab pegol (Cimzia)) within one year prior to initiation and one year post initiation, had evidence of a dispense of any of the included medications prior to the request, or if they did not have a full year of follow-up data. Patients were categorized into groups based on their initial prescription of either adalimumab or etanercept.
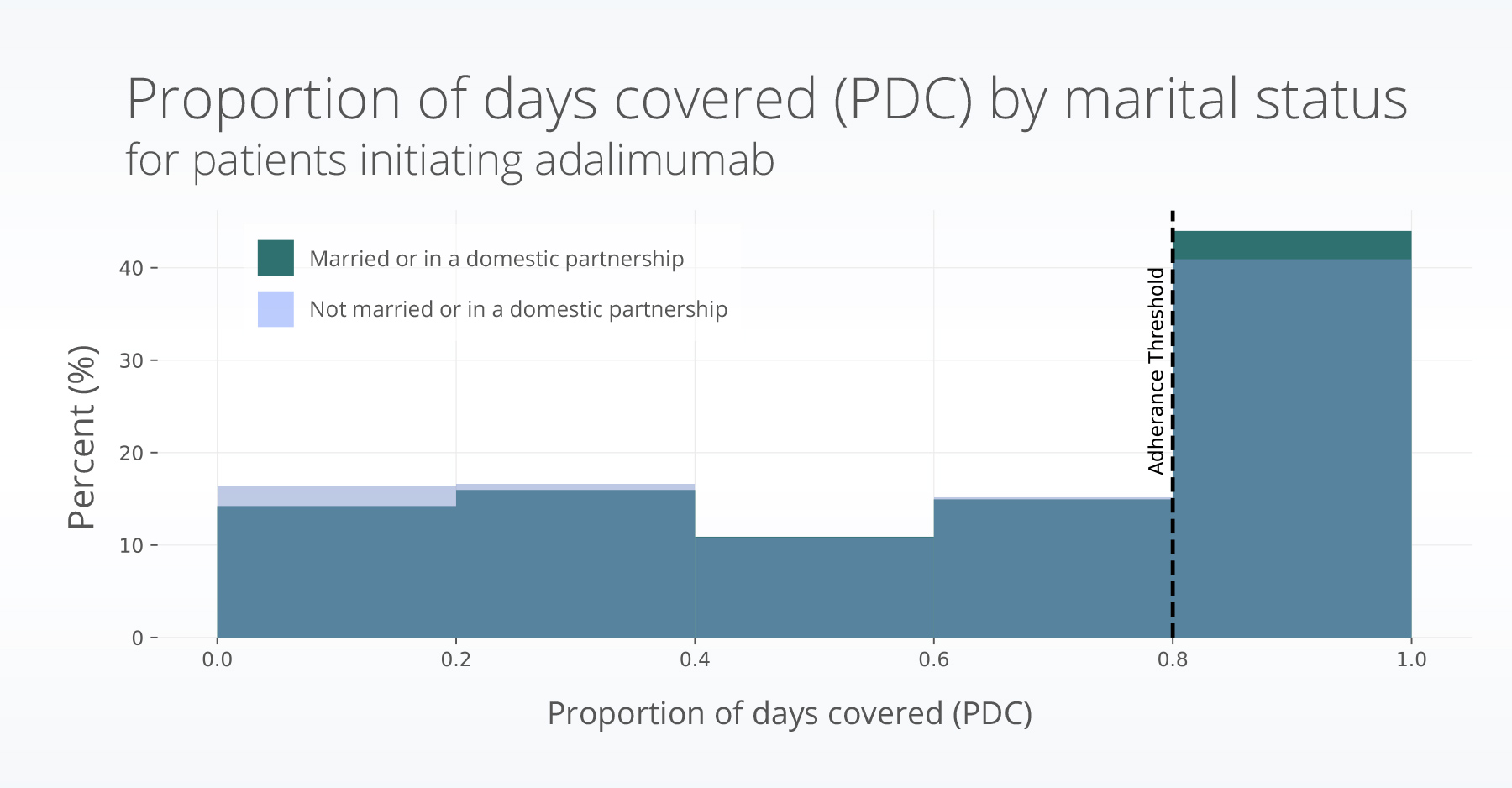
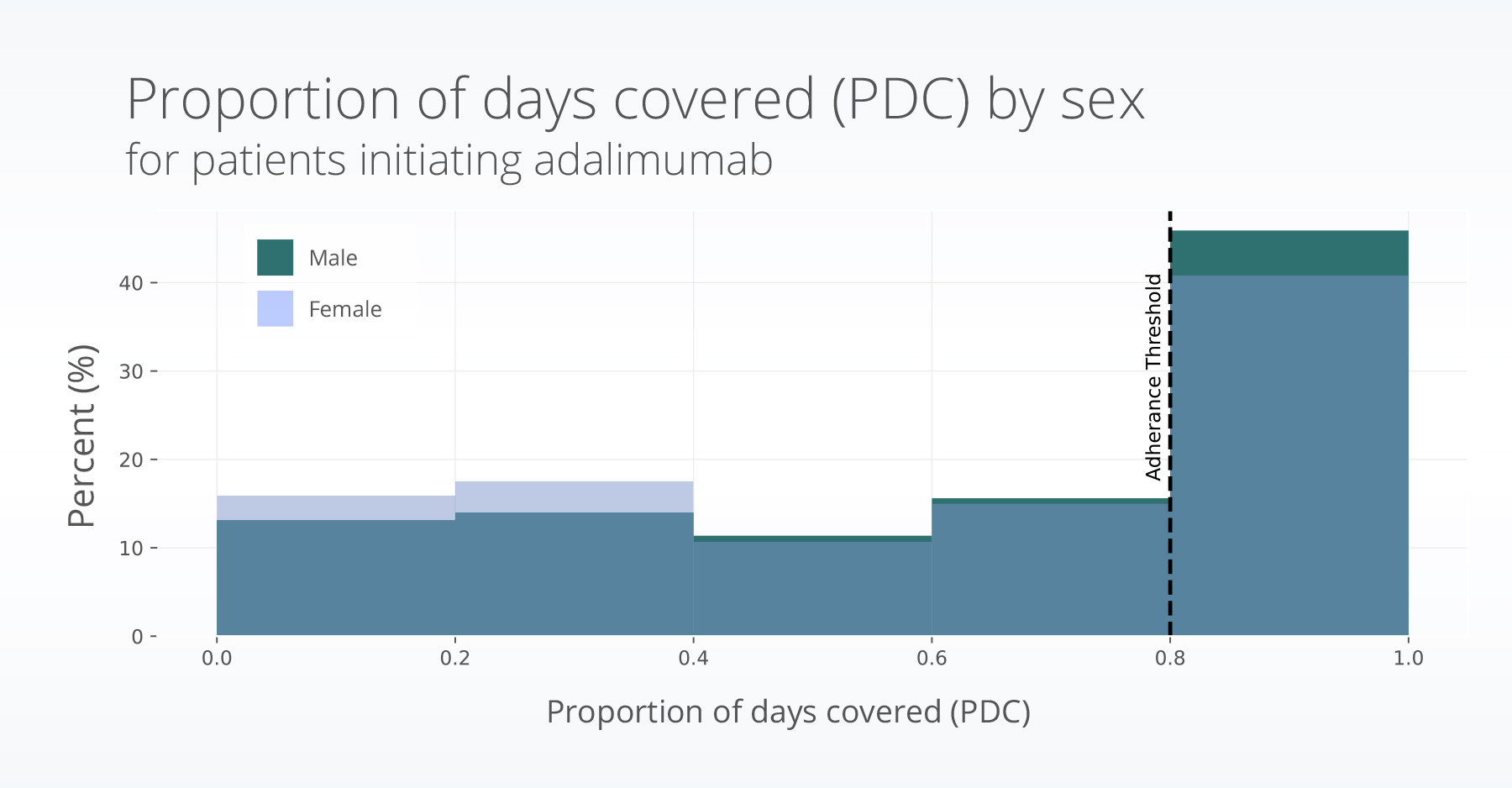
The proportion of days covered (PDC) calculates the percentage of days that a patient had medication on hand during a specified period and is an established metric to assess medication adherence (Centers for Disease Control and Prevention, 2023). It provides insights into the extent patients consistently take their prescribed medications over a specific period. In this study, we calculated the one-year PDC for patients in both groups based on their first treatment initiation (dispense). PDC was calculated by determining the medication supply that was available to patients, which includes the days in each prescription fill, plus any leftover medication from previous fills. The total number of days the patient had medication available to them within the one-year period were calculated (days covered). The percentage of the days covered during a year was then calculated (for more on this, see figure 1 in the first blog in this series about medication adherence). We considered a patient adherent if they had over 80% of their days covered, a common threshold for medication adherence (Ho et al., 2009).
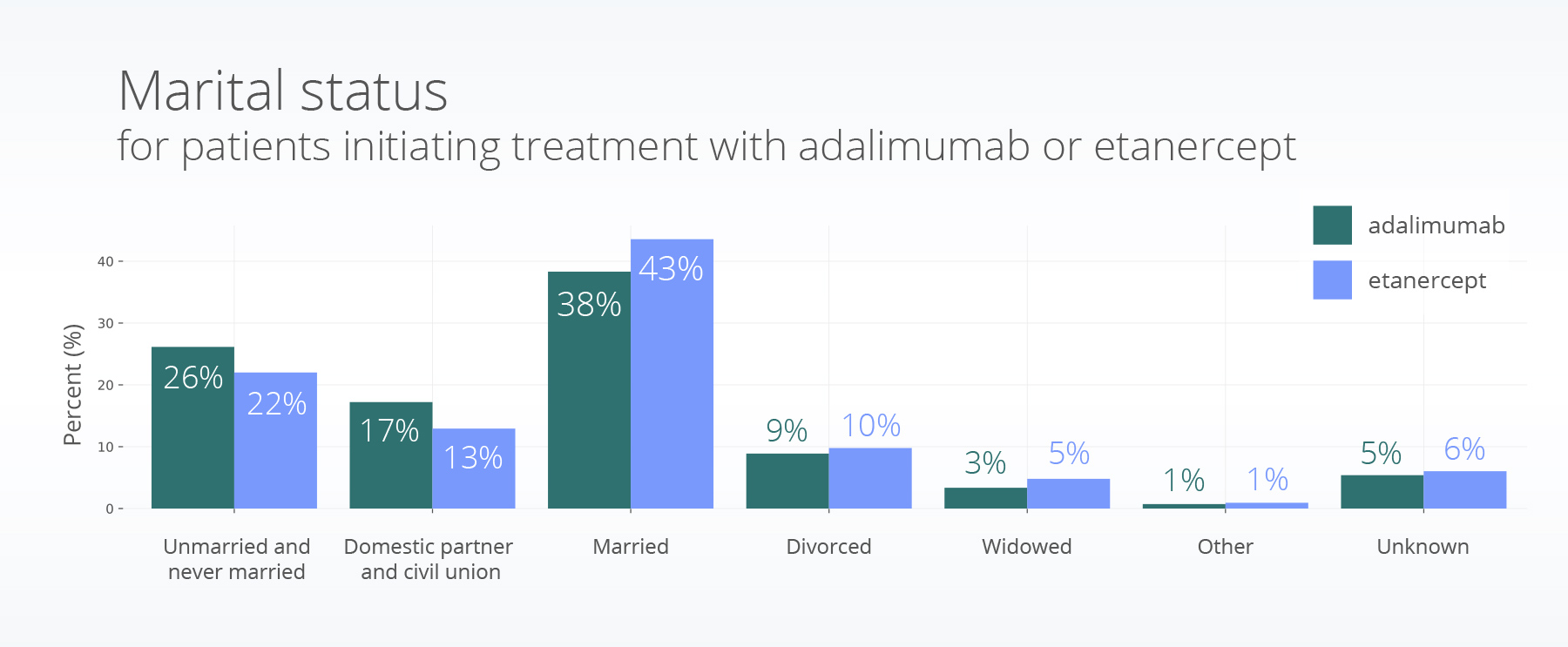
We used logistic regression models to understand the associations of race, ethnicity, age, sex, income, marital status, education, and address stability with PDC, separately for adalimumab and etanercept. We show plots of raw individual income, education, and marriage data; however, in the model, each variable some categories were grouped.
Results
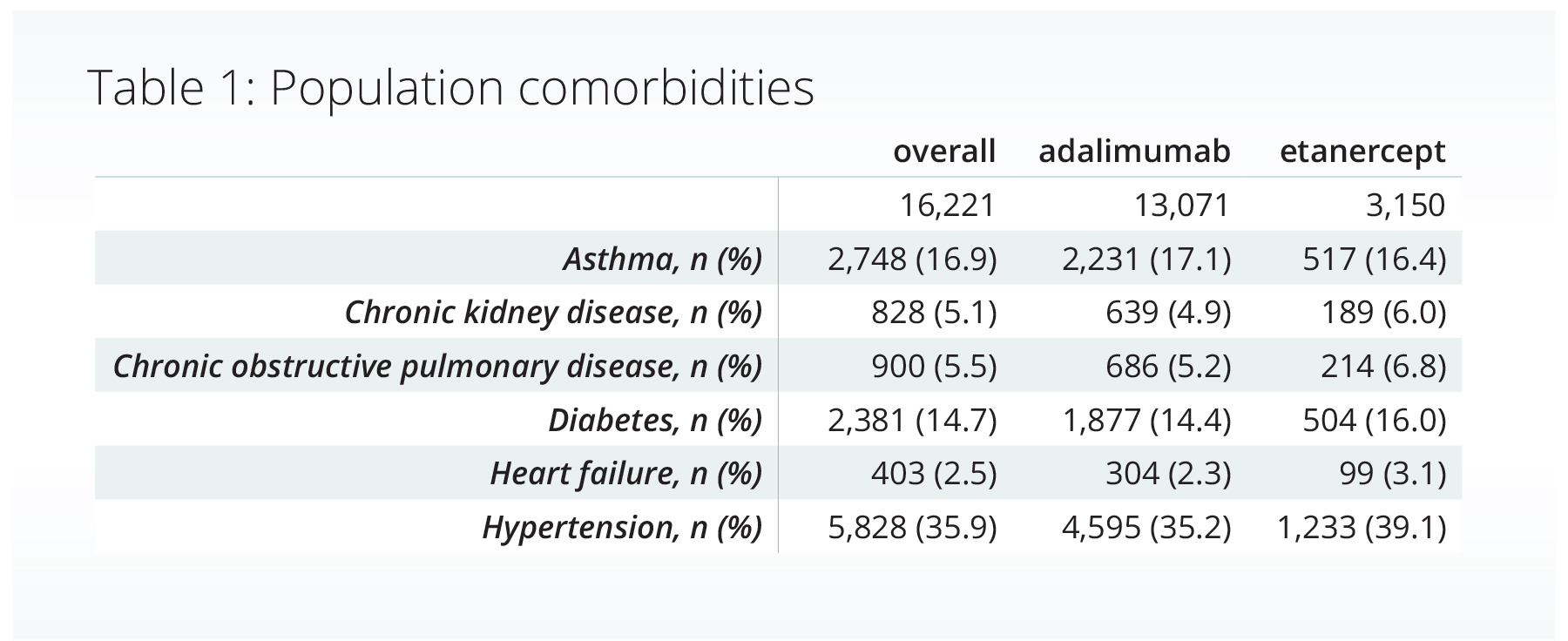
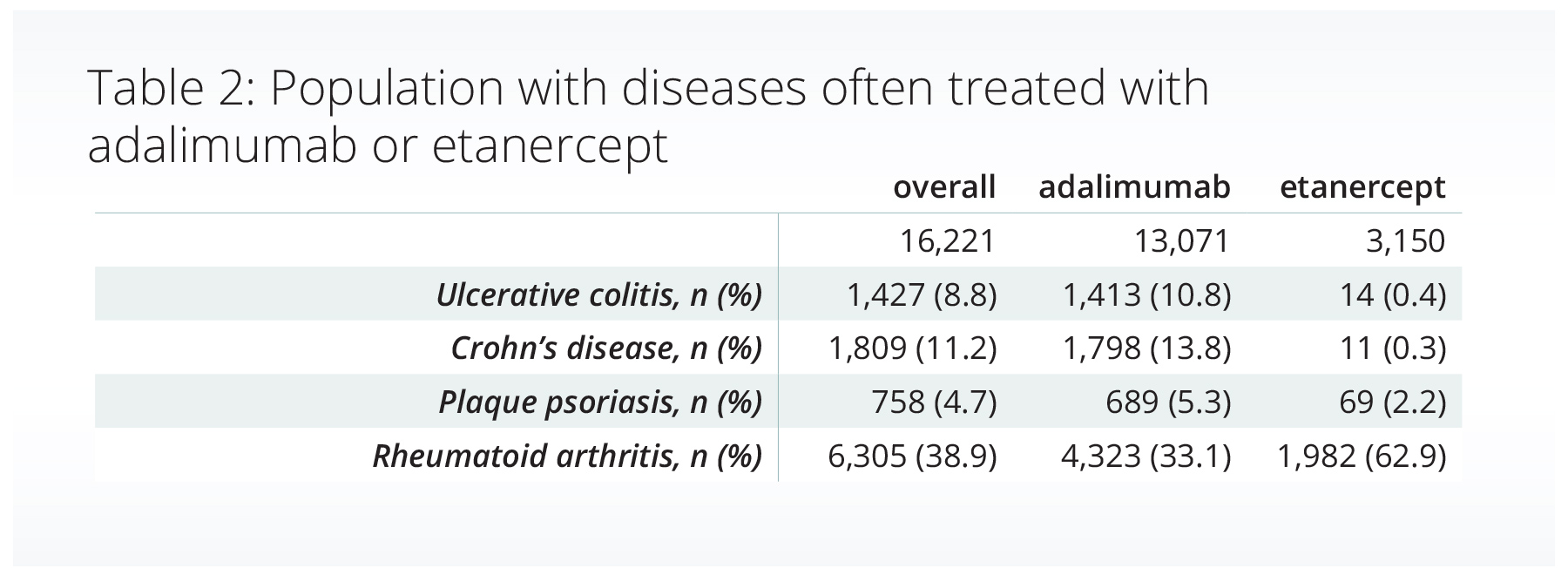
We included over 16,000 adults who initiated treatment with adalimumab or etanercept and met our inclusion criteria. The population was primarily female (66.8%), of white race (81.4%), and not Hispanic or Latino (85.7%). The tables below show the percentage of people with a variety of comorbidities (Table 1) and diseases often treated with adalimumab or etanercept (Table 2, conditions are not mutually exclusive).
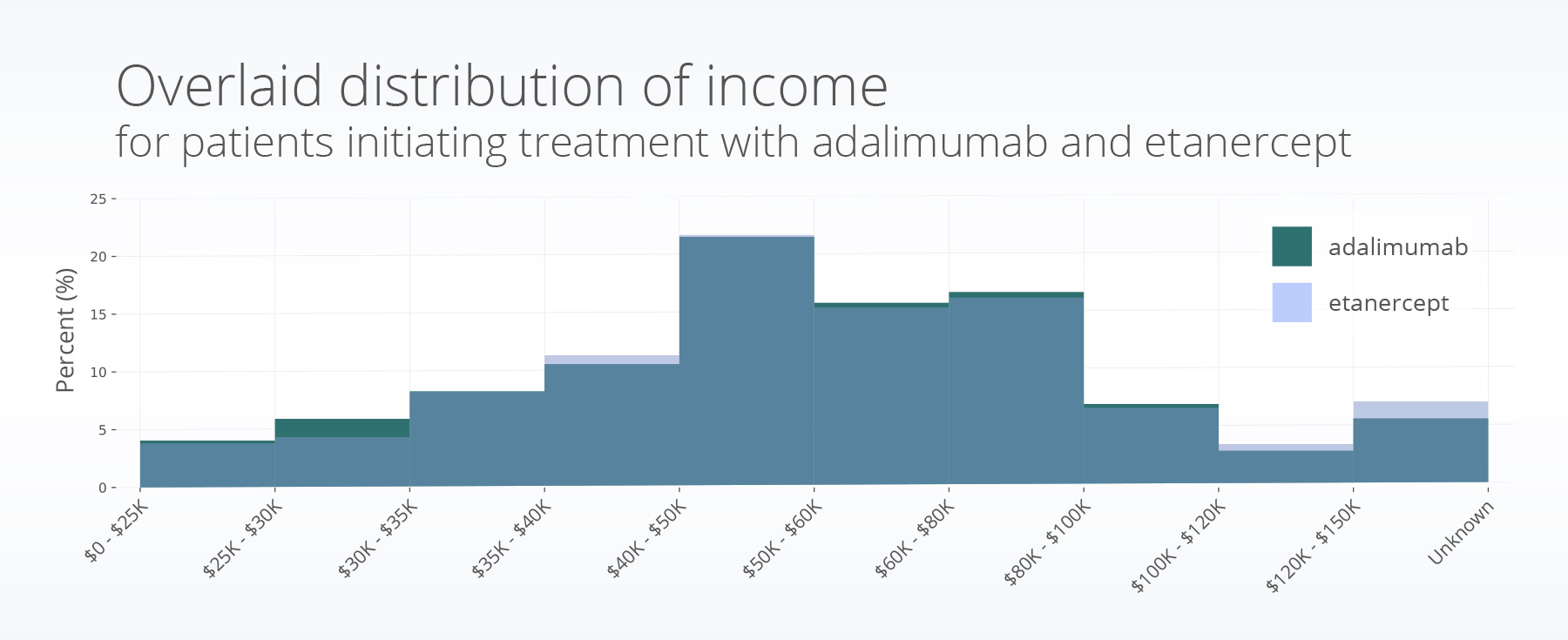
The annual incomes between the two populations follow similar distributions, with a median of $40,001 – 50,000 for adalimumab and $50,001 – 60,000 for etanercept. Both drugs shared the same 25th ($35,001 – 40,000) and 75th percentile ($60,001 – 80,000).
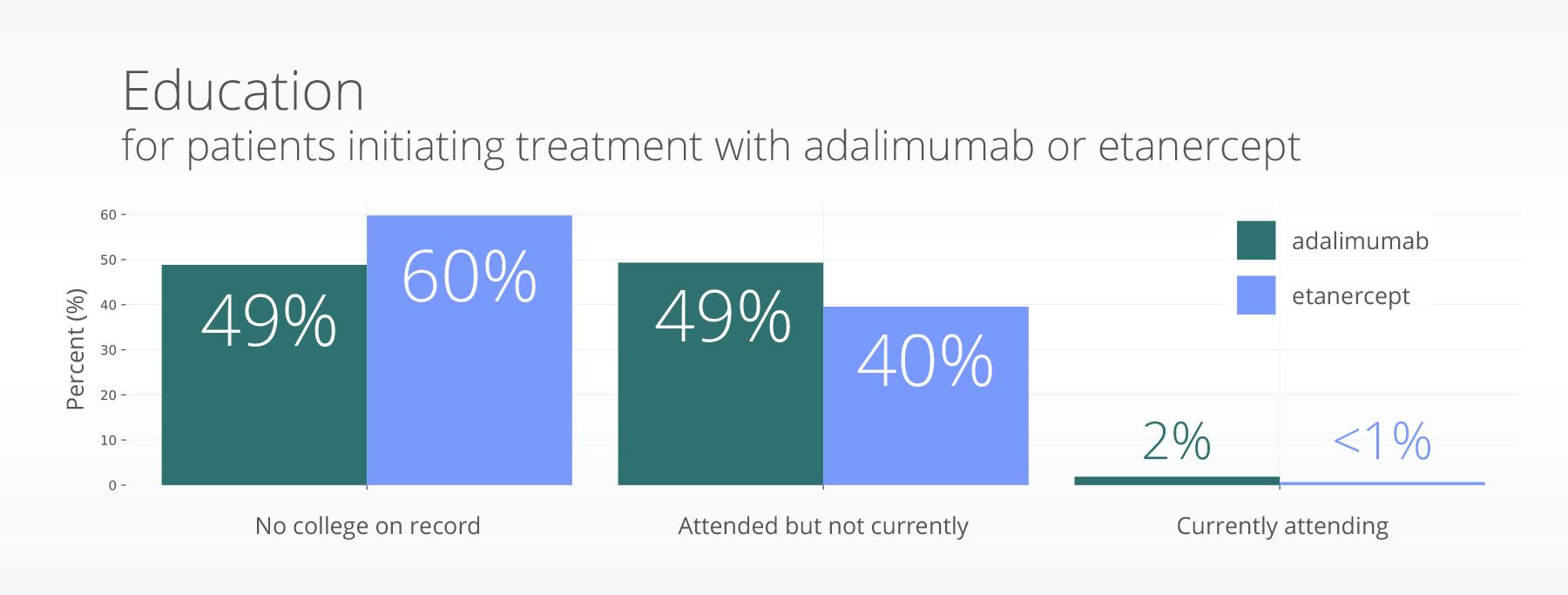
Nearly half of patients initiating adalimumab (48.8%) did not have evidence of attending college; etanercept was even higher at 59.8% with no evidence of college.
Over 50% of both the adalimumab and etanercept populations are married or in a domestic or civil union partnership (a measure of some social support).
Adalimumab medication adherence
Over half the adalimumab group (58%) did not meet the criteria for adherence. Adherence to adalimumab was higher amongst males (OR = 1.24, p<0.001) and people who were married (OR =1.11, p = 0.015), after controlling for other factors. Race, ethnicity, age, income, education, and address stability were not significantly associated with medication adherence.
Etanercept medication adherence
For patients initiating treatment with etanercept, no demographic or SDOH variables included in the model were significantly associated with medication adherence. Over 60% of the population was no adherent to their medication.
Discussion
In our analysis we found low adherence to adalimumab and etanercept for over half of the population. We also found a significant association of increased adherence for males and those who were married in the adalimumab population. This was not seen in the etanercept population. Since such a large population had low adherence there may be additional factors which contribute to an individual’s ability to access these drugs and take them on a regular basis.
In the early 1980’s Roy Penchansky and J. William Thomas published a paper defining the five A’s of access, which have been used since that time to frame a variety of challenges across the healthcare landscape (Penchansky & Thomas, 1981). They define access as availability, accessibility, accommodation, affordability, and acceptability (Penchansky & Thomas, 1981). In this study we only considered affordability (through individual income); however, other factors may influence a person’s ability to regularly adhere to these medications. Examples of this could include: 1) have there been local drugs shortages that may have prevented the ability to regularly get access to these drugs (availability), 2) how easy was it for a patient to get to their pharmacy (accessibility), 3) did pharmacy hours of operation prevent certain people from being able to pick up their prescriptions due to their job or other commitments and for patients taking etanercept did they have use of daily refrigeration for the medication (accommodation), and 4) did the patient understand their diagnosis and feel comfortable with the decisions being made as part of their medical care (acceptability)? Taking all five aspects of access into account gives a more holistic view of potential barriers that may prevent people from adhering to medications.
Although there was low adherence, modifiable barriers to improve medication adherence for all patients may include increased patient education and clarity on prescription instructions/refill steps, especially when changing treatment plans (Fernandez-Lazaro et al., 2019; Taibanguay et al., 2019). Further, patient support groups have also been shown to increase medication adherence (Fendrick et al., 2021). Increasing access to these for all patients without them being a burden could be useful. Additionally, the recent approval of biosimilars for adalimumab are expected to lower cost, which may improve medication adherence for patients taking adalimumab and increase the chance that these medications are included in the drug formulary for more insurance plans. This is an important topic for future study.
Previous studies have compared medication adherence for patients taking drugs to treat rheumatoid arthritis, including adalimumab (Bergman et al., 2023). They found medication adherence to be higher amongst a set of 6,000 patients who were prescribed upadacitinib (Rinvoq) (Bergman et al., 2023). Potentially, this may be due to differences in self-injections versus daily pills.
There are a few limitations with the current analysis. First, the model did not account for patients with different diseases or disease severity. There may be more of an incentive to increase adherence with more severe symptoms. Additionally, we did not include any biosimilars for adalimumab due to the time period studied. Finally, there are additional factors of access which may contribute to differences in medication adherence within these groups.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on September 27, 2023.
Citations
American Heart Association. (2023). Medication Adherence—Taking Your Meds as Directed. https://www.heart.org/en/health-topics/consumer-healthcare/medication-information/medication-adherence-taking-your-meds-as-directed
Bergman, M., Chen, N., Thielen, R., & Zueger, P. (2023). One-Year Medication Adherence and Persistence in Rheumatoid Arthritis in Clinical Practice: A Retrospective Analysis of Upadacitinib, Adalimumab, Baricitinib, and Tofacitinib. Advances in Therapy. https://doi.org/10.1007/s12325-023-02619-6
Centers for Disease Control and Prevention. (2023, February 24). Pharmacy-Based Interventions for Medication Adherence. Search Menu Navigation Menu Division for Heart Disease and Stroke Prevention. https://www.cdc.gov/dhdsp/pubs/medication-adherence.htm
DiMatteo, M. R. (2004). Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis. Health Psychology, 23(2), 207–218. https://doi.org/10.1037/0278-6133.23.2.207
Drugs.com. (2023, August). Enbrel Prices, Coupons and Patient Assistance Programs. https://www.drugs.com/price-guide/enbrel
Drugs.com, & Anderson, L. A. (2023, April 10). How much does Humira cost without insurance? https://www.drugs.com/medical-answers/humira-cost-without-insurance-3537595/
Fendrick, A. M., Macaulay, D., Goldschmidt, D., Liu, H., Brixner, D., Ali, T., & Mittal, M. (2021). Higher Medication Adherence and Lower Opioid Use Among Individuals with Autoimmune Disease Enrolled in an Adalimumab Patient Support Program in the United States. Rheumatology and Therapy, 8(2), 889–901. https://doi.org/10.1007/s40744-021-00309-9
Fernandez-Lazaro, C. I., Adams, D. P., Fernandez-Lazaro, D., Garcia-González, J. M., Caballero-Garcia, A., & Miron-Canelo, J. A. (2019). Medication adherence and barriers among low-income, uninsured patients with multiple chronic conditions. Research in Social and Administrative Pharmacy, 15(6), 744–753. https://doi.org/10.1016/j.sapharm.2018.09.006
Ho, P. M., Bryson, C. L., & Rumsfeld, J. S. (2009). Medication Adherence: Its Importance in Cardiovascular Outcomes. Circulation, 119(23), 3028–3035. https://doi.org/10.1161/CIRCULATIONAHA.108.768986
Jimmy, B., & Jose, J. (2011). Patient Medication Adherence: Measures in Daily Practice. Oman Medical Journal, 26(3), 155–159. https://doi.org/10.5001/omj.2011.38
Osborn, C. Y., Kripalani, S., Goggins, K. M., & Wallston, K. A. (2017). Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients. Journal of Health Care for the Poor and Underserved, 28(1), 499–513. https://doi.org/10.1353/hpu.2017.0036
Penchansky, R., & Thomas, J. W. (1981). The Concept of Access: Definition and Relationship to Consumer Satisfaction. Medical Care, 19(2), 127–140. https://doi.org/10.1097/00005650-198102000-00001
Phillion, M. (2022, May 9). The Impact of Cost on Medication Adherence. Patient Safety & Quality Healthcare. https://www.psqh.com/analysis/the-impact-of-cost-on-medication-adherence/
Taibanguay, N., Chaiamnuay, S., Asavatanabodee, P., & Narongroeknawin, P. (2019). Effect of patient education on medication adherence of patients with rheumatoid arthritis: A randomized controlled trial. Patient Preference and Adherence, Volume 13, 119–129. https://doi.org/10.2147/PPA.S192008
