- Social drivers of health (SDOH), such as increased financial struggles and decreased social support, have been shown to be correlated with decreased medication adherence.
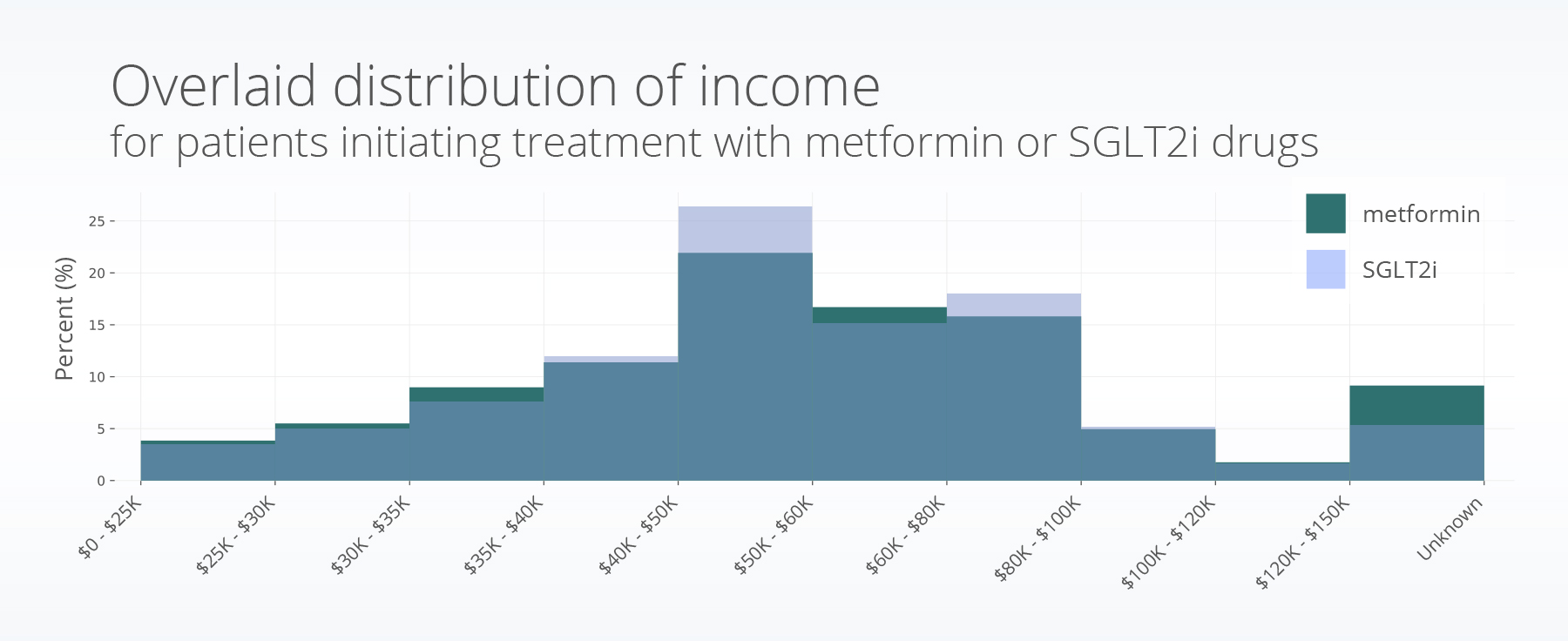
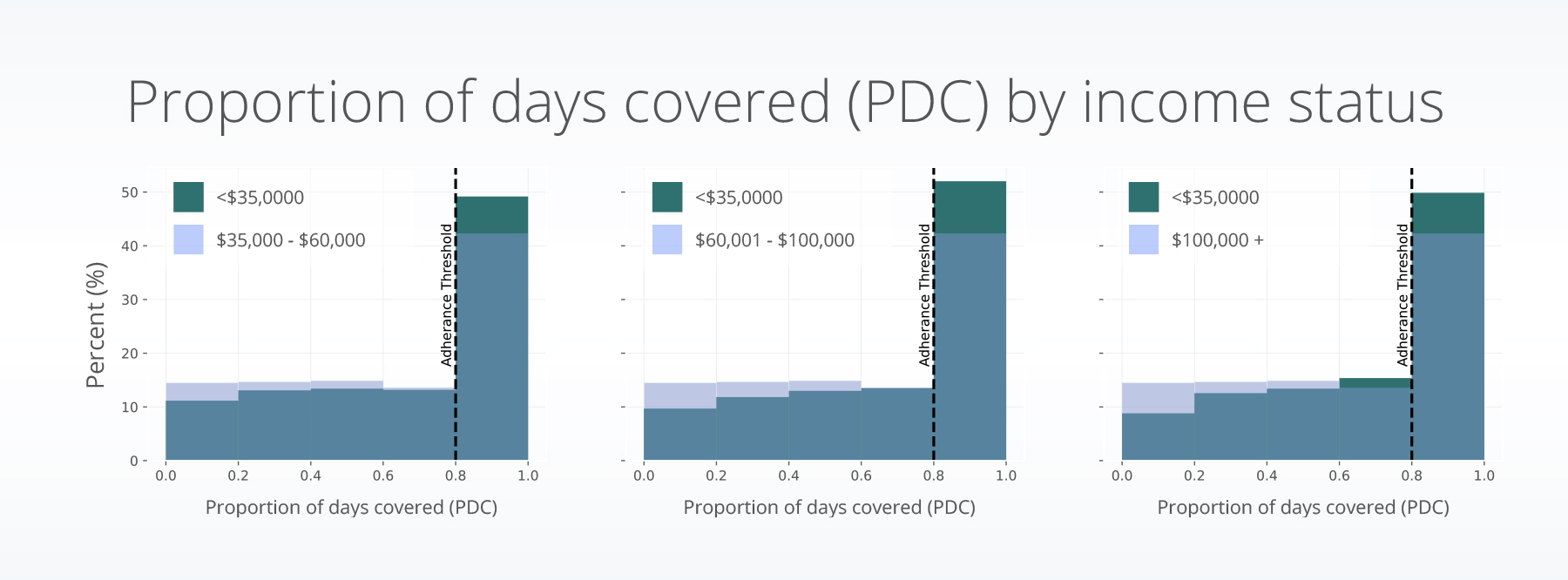
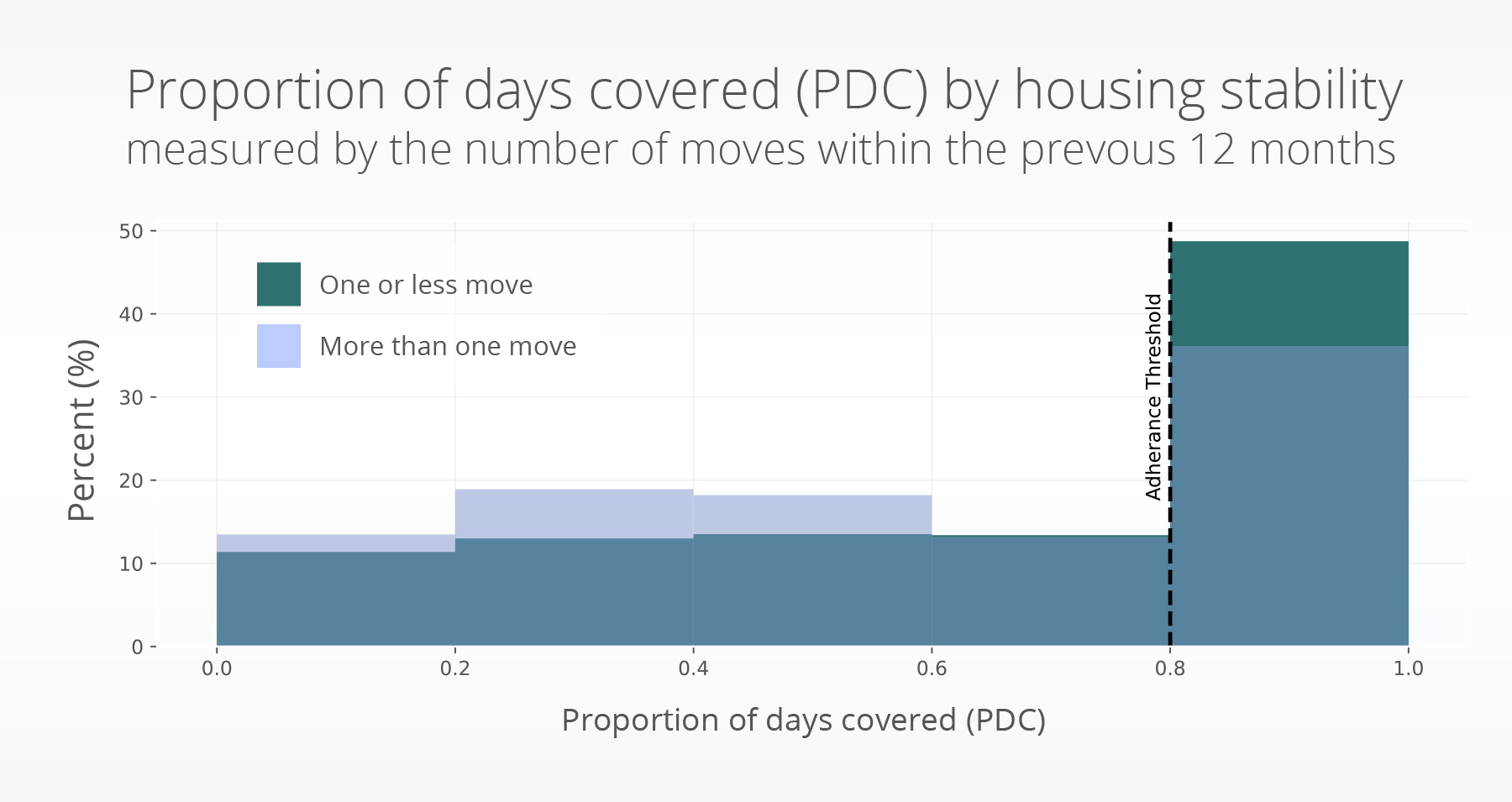
- In this study of patients with type 2 diabetes, we saw an increased rate of medication adherence for those with individual incomes between $35,001 – 100,000 compared to people with incomes below $35,000, for people who were married compared to those who were not, and those who had greater housing stability.
Several previous studies have found associations between certain SDOH factors and medication adherence. For younger populations, lower medication adherence has been associated with lack of health coverage and lower self-management support (Trief et al., 2022). In a population of veterans, lower first-year adherence was associated with never being married or being divorced/separated (Gatwood et al., 2018). Additionally, increased income has been shown to be associated with increased medication adherence for the medication metformin (Huang et al., 2022). Further, survey results showed a connection between financial hardship from medical bills, higher comorbidity burden, and female sex were associated with cost-related medication nonadherence (Caraballo et al., 2020).
Therefore, we were interested in understanding differences in first-year medication adherence rates between metformin and SGLT2i medications accounting for SDOH variables.
Methods
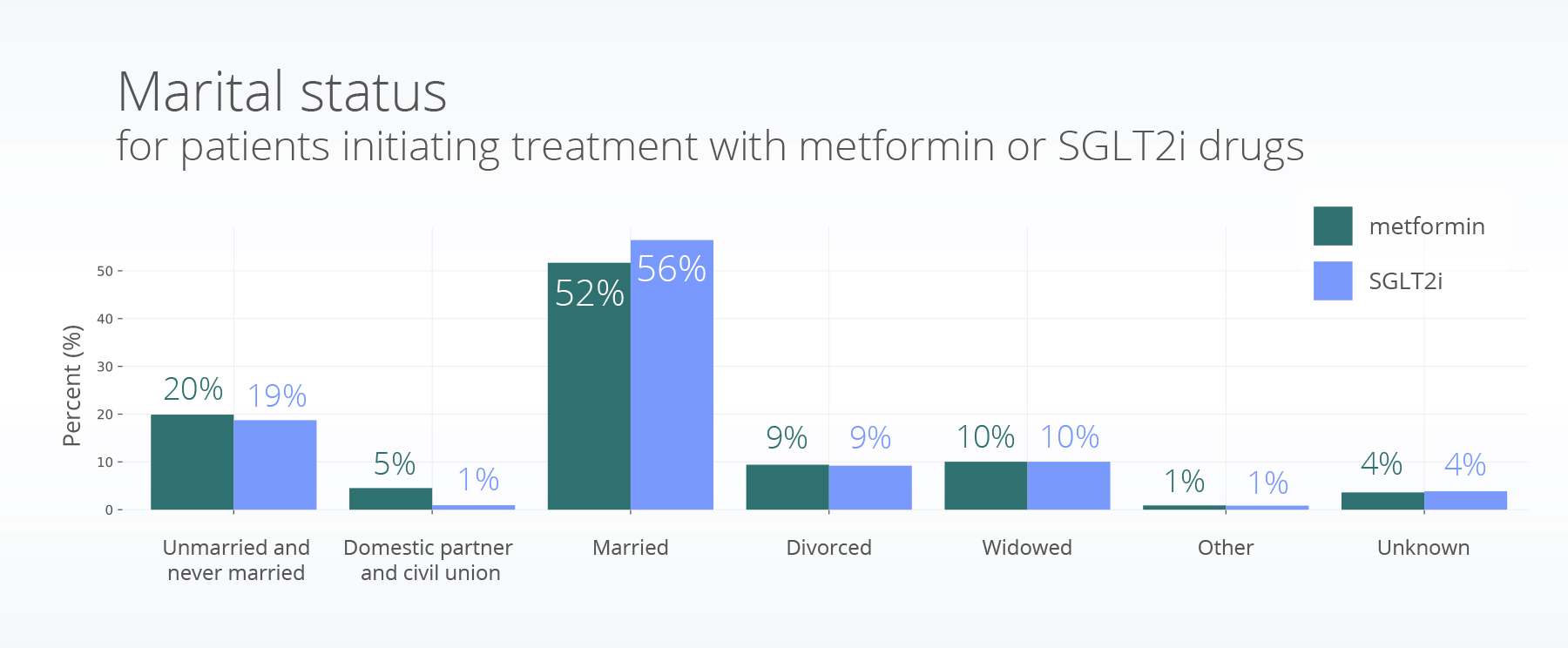
People were excluded if they were less than 18 years old at the time of their first prescription, received a prescription or dispense for any of the other medications in the study within one year after initiation, had evidence of a dispense of any of the included medications prior to the request, or if they did not have a full year of follow-up data. Patients were categorized into groups based on their initial prescription of either an SGLT2i or metformin.
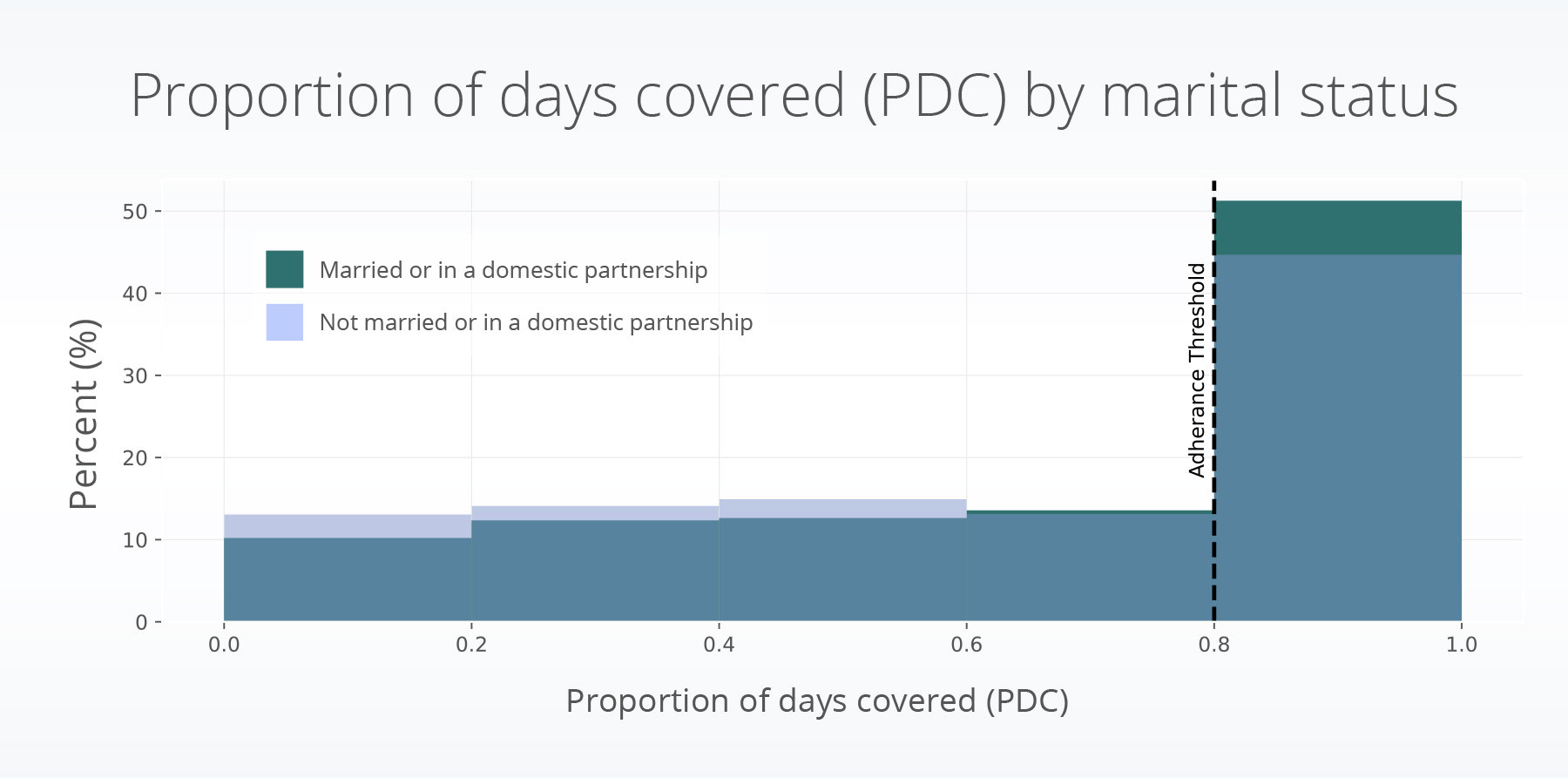
The proportion of days covered (PDC) calculates the percentage of days that a patient had medication on hand during a specified period and is an established metric to assess medication adherence (Centers for Disease Control and Prevention, 2023). It provides insights into the extent patients consistently take their prescribed medications over a specific period. In this study, we calculated the one-year PDC for patients in both groups based on their first treatment initiation (dispense). PDC was calculated by determining the medication supply that was available to patients, which includes the days in each prescription fill, plus any leftover medication from previous fills. The total number of days the patient had medication available to them within the one-year period were calculated (days covered). The percentage of the days covered during a year was then calculated (for more on this, see figure 1 in the first blog in this series about medication adherence). We considered a patient adherent if they had over 80% of their days covered, a common threshold for medication adherence (Ho et al., 2009).
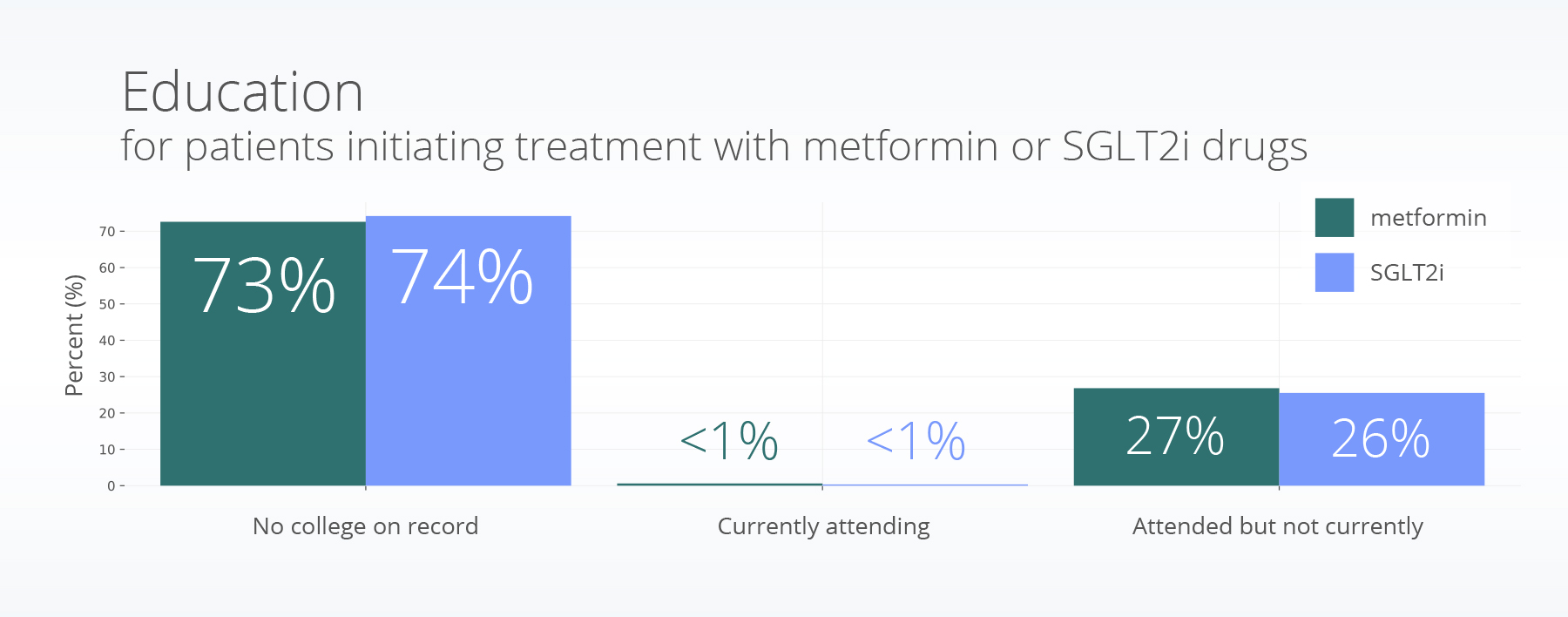
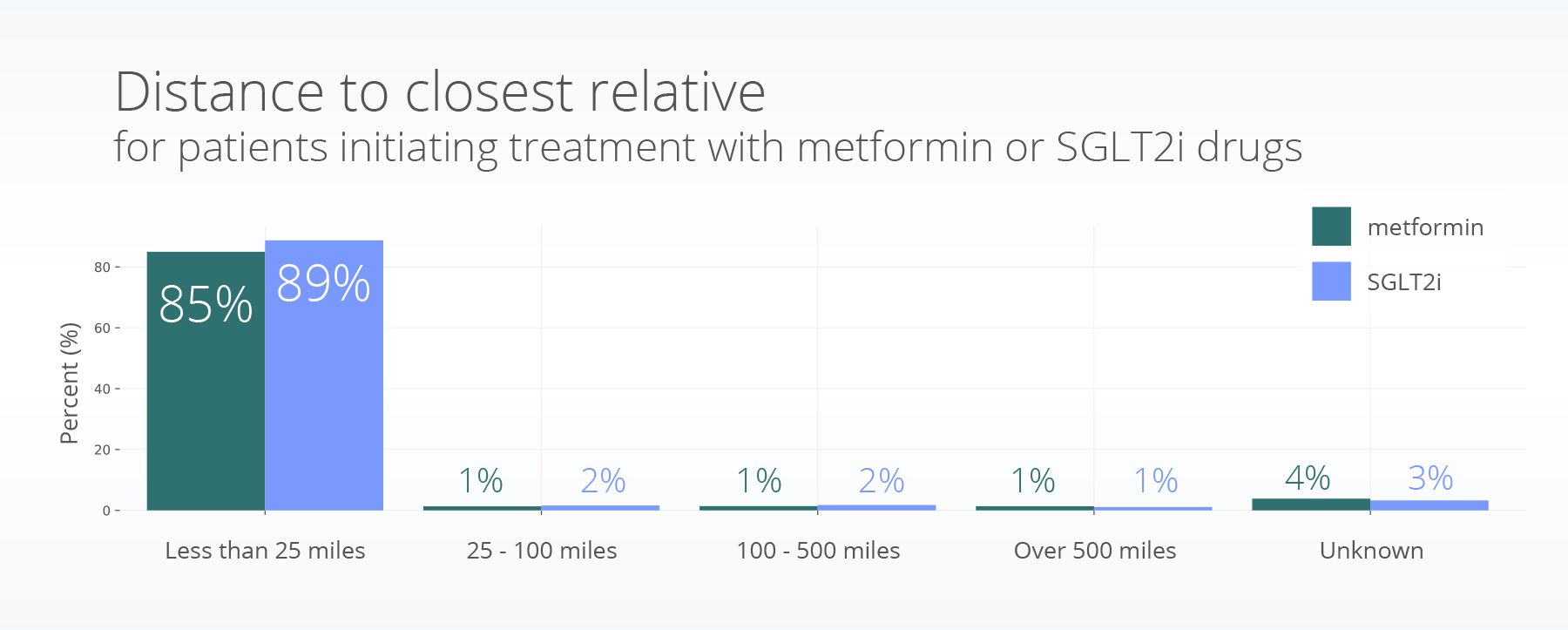
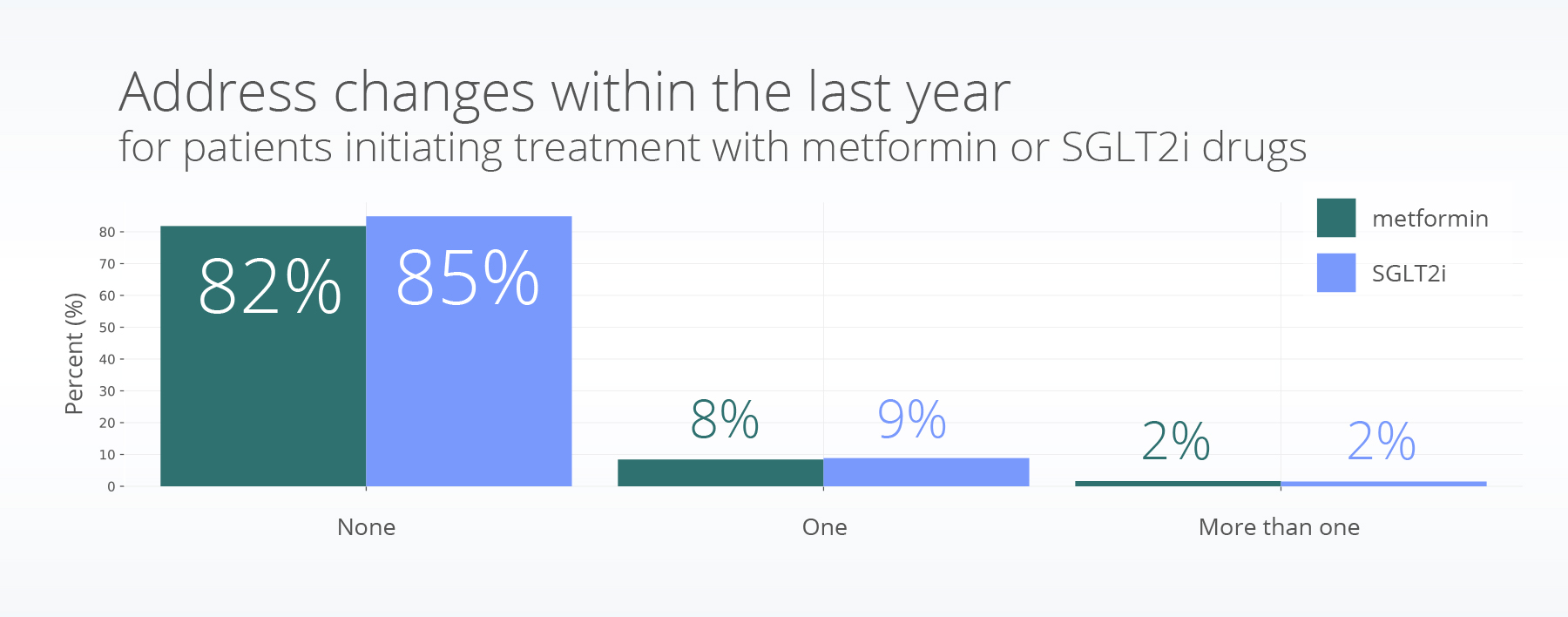
We used a logistic regression model to understand differences between people who were adherent compared to those who were not adherent. The model included treatment group, age, race, sex, ethnicity, and SDOH factors of income, education, marital status, distance to closest family relative, and housing stability (measured by the number of moves in the last 12 months). We tested for associations between SDOH and medication adherence.
Results
Similar to the results of our previous insight, we saw higher medication adherence for males (OR = 1.07, p=0.001), patients who were white (Black or African American: OR = 0.58, p<0.001, Asian: OR = 0.87, p = 0.016, American Indian or Alaska Native: OR = 0.55 p =0.004, Native Hawaiian or Other Pacific Islander: OR = 0.69, p =0.45), and those not of Hispanic or Latino ethnicity (OR = 1.47, p <0.001).
Adherence was lower for those who were not married, compared to those who were married or in a domestic partnership (OR = 0.84, p <0.001).
Discussion
A second SDOH variable of interest is social support or being supported physically or emotionally by family, friends, co-workers and others when you need them (CMHA BC & Anxiety Canada, 2016; Towey, 2023) . We used a proxy of marriage and distance to closest relative to investigate one aspect of social support. In this study, we saw different medication adherence for people who were married compared to those who were not, but we did not see a difference in distance to closest relative. The categories for this variable include less than 25 miles, 25-100 miles, 100-500 miles, and over 500 miles; these categories may not be detailed enough to distinguish social support in this way.
As a proxy for housing stability, we included a variable of having more than one move within the last 12 months; we saw a lower rate of adherence for people who have moved more than once in the prior year. A study of people with HIV found similar trends and associated them with difficulty storing medications, inconsistent and disruptive access to healthcare and resources, and competing physical and mental health needs (Fernandez et al., 2022). More research is needed to understand if similar factors may be at play in this population. Finally, we included college education as an SDOH variable because education tends to be a predictor of medication access and adherence; however, we did not see any significant associations in this study.
There are a few limitations with this study. We outlined limitations about studying SGLT2i and metformin in our previous blog (e.g., differences in treatment recommendations, medication availability, side effects / additional benefits, costs for metformin vs. SGLT2i, etc.), and additional relevant details are available in part 1 of the series. Those same limitations hold true for this study as well. Further, there are other SDOH measures, such as patient education of prescriptions, inconsistent work schedules, insurance status, and food stability that may affect medication adherence and were not included here. Specifically, people who are uninsured or on Medicaid may make up a large percentage of the population with incomes under $35,000. This may affect adherence due to no insurance (requiring full payment of the medications) or low and inconsistent coverage of the medications.
In this insight, we showed the rates of medication adherence for two commonly prescribed drug classes for people with type 2 diabetes. Differences in adherence by SDOH may be exacerbated by high-cost specialty drugs. More research is needed here.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on September 15, 2023.
Citations
CMHA BC, & Anxiety Canada. (2016). Metal Health. Welness Module 3: Social Support. https://www.heretohelp.bc.ca/wellness-module/wellness-module-3-social-support
Fernandez, S. B., Lopez, C., Ibarra, C., Sheehan, D. M., Ladner, R. A., & Trepka, M. J. (2022). Examining Barriers to Medication Adherence and Retention in Care among Women Living with HIV in the Face of Homelessness and Unstable Housing. International Journal of Environmental Research and Public Health, 19(18), 11484. https://doi.org/10.3390/ijerph191811484
Gatwood, J. D., Chisholm-Burns, M., Davis, R., Thomas, F., Potukuchi, P., Hung, A., & Kovesdy, C. P. (2018). Disparities in Initial Oral Antidiabetic Medication Adherence Among Veterans with Incident Diabetes. Journal of Managed Care & Specialty Pharmacy, 24(4), 379–389. https://doi.org/10.18553/jmcp.2018.24.4.379
Huang, C. X., Turk, N., Ettner, S. L., Mangione, C. M., Moin, T., O’Shea, D., Luchs, R., Chan, C., & Duru, O. K. (2022). Does the diabetes health plan have a differential impact on medication adherence among beneficiaries with fewer financial resources? Journal of Managed Care & Specialty Pharmacy, 28(9), 948–957. https://doi.org/10.18553/jmcp.2022.28.9.948
Lindenfeld, J., & Jessup, M. (2017). ‘Drugs don’t work in patients who don’t take them’ (C. Everett Koop, MD, US Surgeon General, 1985): Editorial comment. European Journal of Heart Failure, 19(11), 1412–1413. https://doi.org/10.1002/ejhf.920
Quealy, K., & Sanger-Katz, M. (2019, February 7). The Prescription Drugs That Rich People Buy. https://www.nytimes.com/2019/02/07/upshot/income-strong-predictor-drug-purchases-serious-diseases.html
Towey, S. (2023). Taking charge of your health & wellbeing. Social Support. https://www.takingcharge.csh.umn.edu/social-support
Trief, P. M., Kalichman, S., Uschner, D., Tung, M., Drews, K. L., Anderson, B. J., Fette, L. M., Wen, H., Bulger, J. D., & Weinstock, R. S. (2022). Association of psychosocial factors with medication adherence in emerging adults with youth‐onset type 2 diabetes: The i Count study. Pediatric Diabetes, 23(8), 1695–1706. https://doi.org/10.1111/pedi.13431
