- Annually, over 125,000 deaths are associated with poor medication adherence. The proportion of days covered (PDC) is a common method to measure adherence.
- When controlling for age, sex, race, and ethnicity, we found similar rates of first year medication adherence for people newly initiating metformin or drugs in the SGLT2i class.
Sodium glucose cotransport 2 inhibitors (SGLT2i) and metformin are medications used to lower blood sugar for people with type 2 diabetes. While both types of medications are effective, medication adherence is key to their success. Medication adherence refers to the extent to which a patient takes their medication as prescribed by their healthcare provider, but unfortunately, an estimated 125,000 deaths occur every year in the US due to poor medication adherence (American Heart Association, 2023). Therefore, studying medication adherence trends for these medications could help to improve patient care and outcomes.
A number of factors may lead to differences in adherence between SGLT2i and metformin, including the higher cost of SGLT2i, higher dose frequency for some forms of metformin, different side effects, and additional positive benefits, such as weight loss and kidney function from SGLT2i (Cowie & Fisher, 2020).
We set out to understand if there were differences in medication adherence rates between patients first initiating an SGLT2i drug or metformin.
Methods
Looking at a subset of Truveta Data, we identified people who initiated treatment for an SGLT2i (i.e., dapagliflozin (Farxiga), empagliflozin (Jardiance), canagliflozin (Invokana), or ertugliflozin (Steglatro)) or metformin between January 2016 and September 2023. Treatment initiation was defined as a first-time prescription and a dispensed medication within 60 days.
People were excluded if they were less than 18 years old at the time of their first prescription, they received a prescription or dispense for any of the other drugs in the study within one year, they had evidence of a dispense of any of the drugs prior to the request, or they did not have a full year of dispense data. Patients were categorized into treatment groups based on their initial prescription of either an SGLT2i or metformin.
The proportion of days covered (PDC) calculates the percentage of days that a patient had medication on hand during a specified period and is an established metric to assess medication adherence (Centers for Disease Control and Prevention, 2023). It provides insights into the extent patients consistently take their prescribed medications over a specific period. In this study, we calculated the one-year PDC for patients in both groups based on their first treatment initiation (dispense). PDC was calculated by determining the medication supply that was available to patients, which includes the days in each prescription fill, plus any leftover medication from previous fills. The total number of days the patient had medication available to them within the one-year period were calculated (days covered). The percentage of the days covered during a year was then calculated (Figure 1). We considered a patient adherent if they had over 80% of their days covered, a common threshold (Ho et al., 2009).
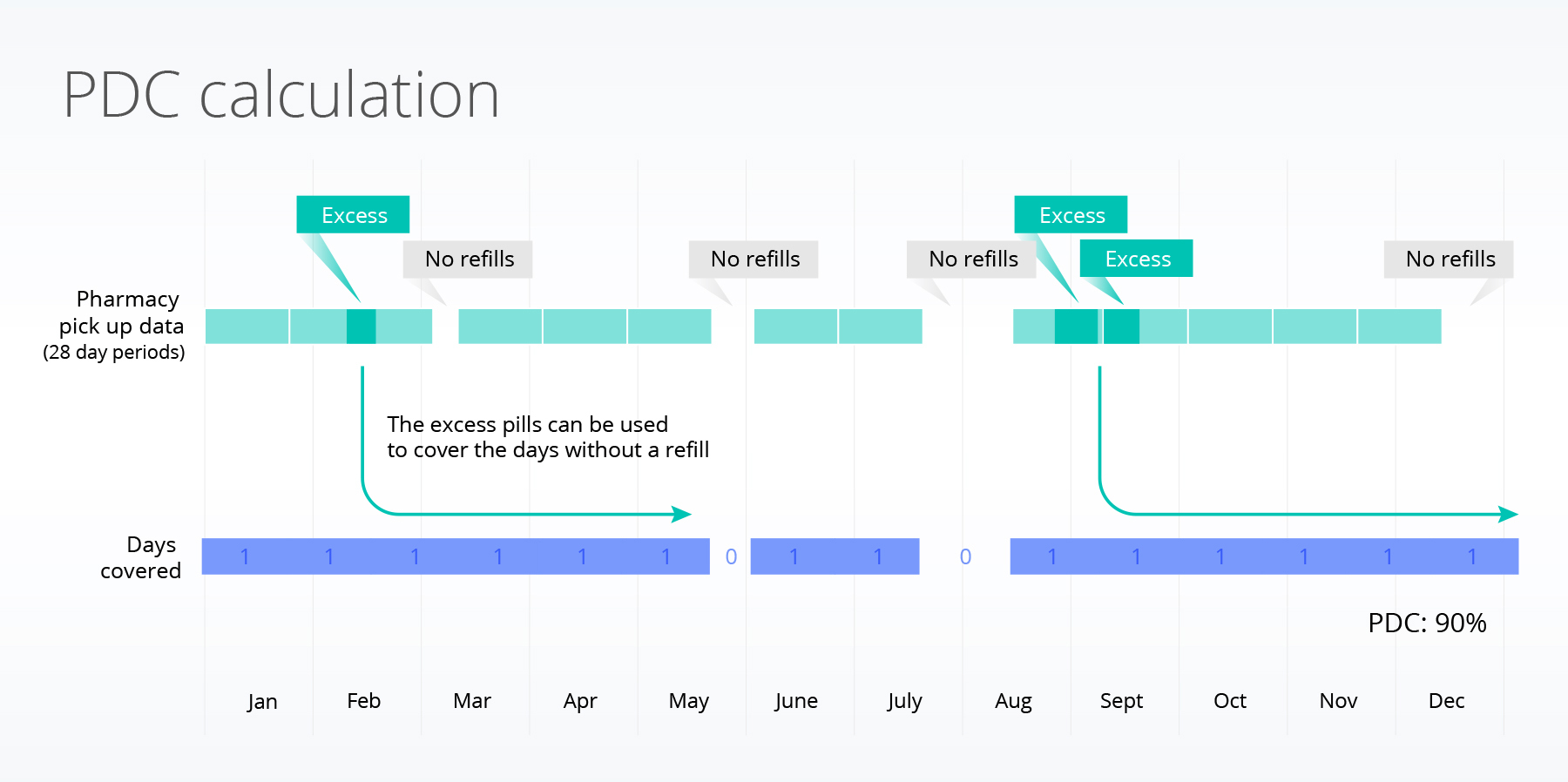
Figure 1: Calculating the proportion of days covered (PDC). Each of the green boxes represents a 28-day dispense of an SGLT2i or metformin. To be fully adherent to a medication, a patient needs to receive a refill every 28 days. Sometimes people receive refills early (resulting in excess) or do not refill when they end a current prescription. The excess can be used to cover any prescription caps. The blue shows the days that are covered. Gaps (shown in white) occur when a patient has not received a refill and has no excess. The metric calculates the proportion of days covered within one year.
We used a logistic regression model to understand differences between people who were adherent compared to those who were not adherent. The model took into account age, race, sex, and ethnicity. We tested for differences between those initiating metformin and SGLT2i.
Results
We included over 50,000 individuals who initiated treatment with an SGLT2i or metformin. The majority of the population initiated treatment with metformin (~97.6%) and was over 55 years of age. A higher proportion of the SGLT2i population was between 75-85 years of age (10.6% for metformin, compared to 14.1% for SGLT2i) and of Black or African American (henceforth referred to as Black) race compared to the metformin population (14.4% for metformin, compared to 18.1% for SGLT2i).
Overall, only 47.8% of the population met the requirement of more than 80% of days covered.
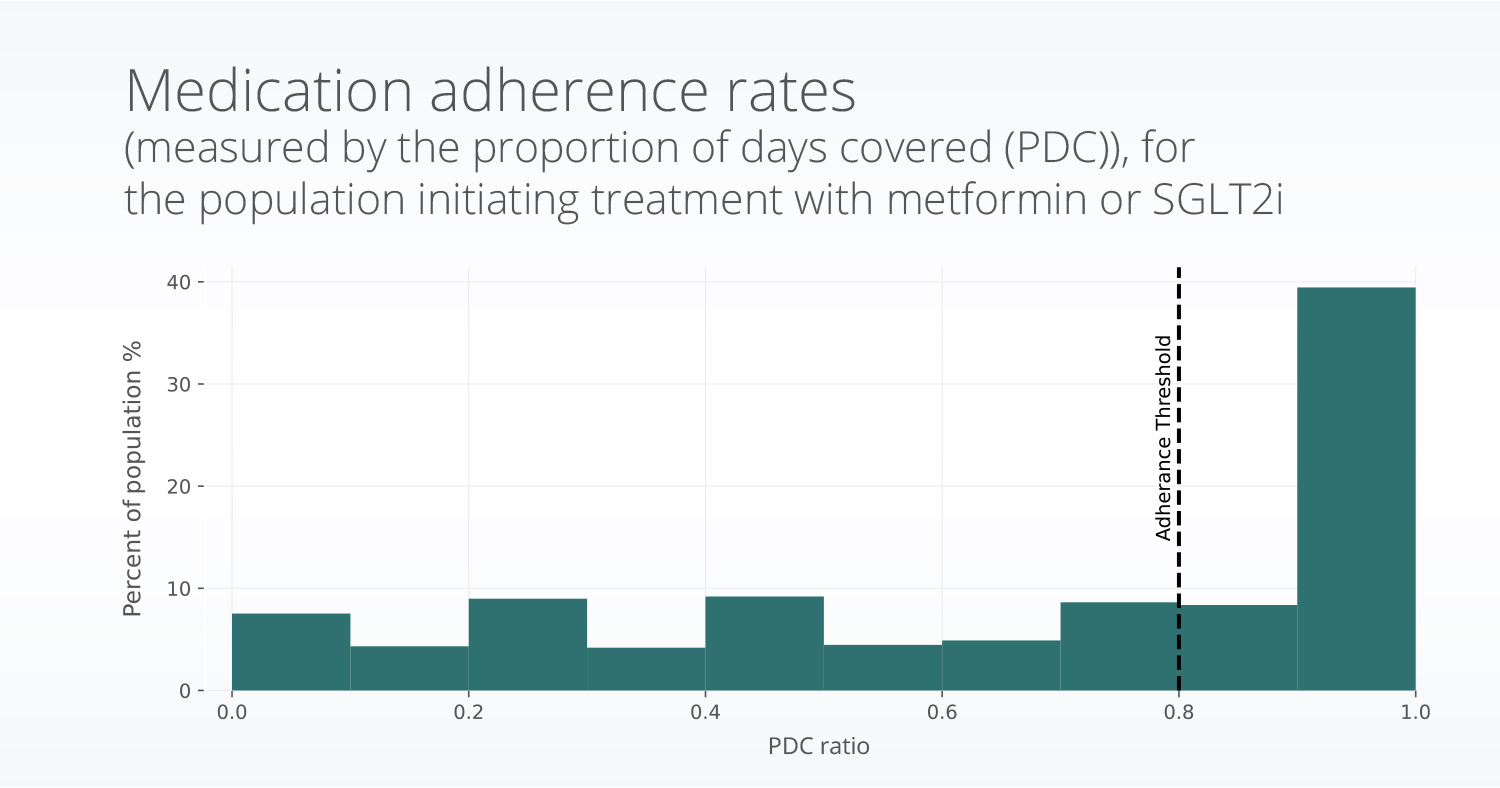
Figure 2: A histogram showing the distribution of medication adherence values for patients in the study.
Odds ratios (OR) are a common way to compare the chance of something happening between two groups. If the odds ratio is 1 it means the two groups have equal odds of something occurring. If the odds ratio is 2, it means the odds of something occurring are 2x as likely in one group than the other group.
When taking into account age, sex, race, and ethnicity, patients initiating SGLT2i had similar adherence to those initating metrormin. Patients of Black (OR: 0.57, p<0.001 ), American Indian or Alaska Native (OR=0.60, p=0.004), and Native Hawaiian or Other Pacific Islander (OR = 0.64, p = 0.012) races were less likely to be adherant compared to patients of white race. Differences were not seen for patients of Asian race, compared to white race. Patients of Non-Hispanic or Latino ethnicity were more likely to be adherent (OR = 1.49, p<0.001). Finally, increased age (p <0.001) and male sex (OR = 1.12, p < 0.001) were assocatied with increased adherance.
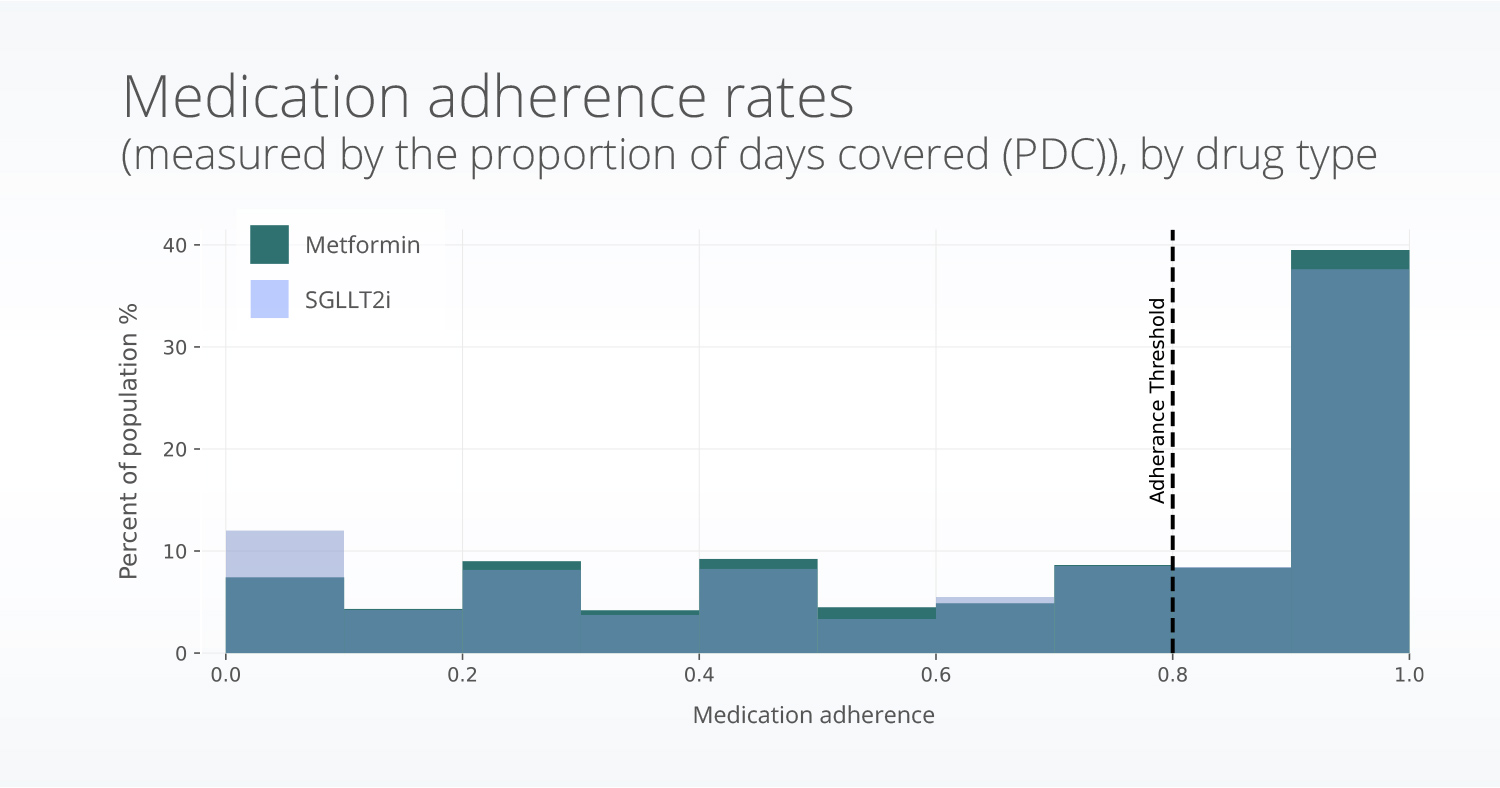
Figure 3: Variation in the medication adherence values by type of drug (SGLT2i or metformin).
Discussion
Medication adherence is critical to achieving full treatment effectiveness and thus helping to manage the disease. Understanding differences in adherence to certain drugs and working to mitigate potential barriers can improve outcomes and increase quality of life. In this study, we specifically looked at potential differences in adherence between SGLT2i drugs and metformin. We found similar one-year adherence for people initiating treatment with SGLT2i and metformin. Previous research has also shown that for antidiabetic medications, the highest rates of adherence were for metformin, followed by SGLT2i (Lee & Lee, 2022). Our results were similar; however, we did not see significant differences between these groups. Another previous study looked at a population of veterans has also showed higher rate of adherence for white individuals compared to people of Black or African American, Native American, or Hawaiian/Pacific Islander races (Gatwood et al., 2018). The results of our study are similar to these.
Metformin is the recommended first-line treatment for most patients with T2D and is prescribed as a first-line treatment more often than SLGT2i drugs (Chen et al., 2020). SGLT2i are typically prescribed when metformin is not able to achieve glycemic control indicating the patient may have a more complex disease state and may be taking additional drugs; both of these factors may contribute to any difference seen in these populations. However, in recent years SGLT2i are increasingly prescribed as first-line agents (Grunberger, 2021; Shin et al., 2022). If SGLT2i medications continue to increase in usage as first-line treatment, this study should be re-run to confirm the results.
There are a few limitations associated with this study; first, as metformin is the recommended first-line treatment and we measured one-year PDC for people with first-time prescriptions of metformin or SGLT2i, the metformin population was much larger than the SGLT2i population. Additionally, metformin has been approved for >25 years, is inexpensive, and has well-understood side effects, whereas SGLT2i are newer and more expensive medications. In addition, SGLT2i can be prescribed for conditions other than type 2 diabetes, such as chronic kidney disease and heart failure (we have previously reported on prescription trends in two SGLT2i medications by disease type). Therefore, patients initiating treatment with SGLT2i may be different from those initiating metformin. We also only included people receiving monotherapies (i.e., therapy paths where one drug was prescribed), although some people are prescribed these medications in combination.
Previous research has connected medication adherence with a variety of social determinants of health factors such as social support, income, and access to resources (Gatwood et al., 2018; Huang et al., 2022; Trief et al., 2022). Additional research is needed to understand if those factors may be connected to the difference in adherence between these populations, which we plan to share in follow-up blogs.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on September 15, 2023.
Citations
American Heart Association. (2023). Medication Adherence—Taking Your Meds as Directed. https://www.heart.org/en/health-topics/consumer-healthcare/medication-information/medication-adherence-taking-your-meds-as-directed
Centers for Disease Control and Prevention. (2023, February 24). Pharmacy-Based Interventions for Medication Adherence. Search Menu Navigation Menu Division for Heart Disease and Stroke Prevention. https://www.cdc.gov/dhdsp/pubs/medication-adherence.htm
Chen, T.-H., Li, Y.-R., Chen, S.-W., Lin, Y.-S., Sun, C.-C., Chen, D.-Y., Mao, C.-T., Wu, M., Chang, C.-H., Chu, P.-H., & Wu, V. C.-C. (2020). Sodium-glucose cotransporter 2 inhibitor versus metformin as first-line therapy in patients with type 2 diabetes mellitus: A multi-institution database study. Cardiovascular Diabetology, 19(1), 189. https://doi.org/10.1186/s12933-020-01169-3
Cowie, M. R., & Fisher, M. (2020). SGLT2 inhibitors: Mechanisms of cardiovascular benefit beyond glycaemic control. Nature Reviews Cardiology, 17(12), 761–772. https://doi.org/10.1038/s41569-020-0406-8
Gatwood, J. D., Chisholm-Burns, M., Davis, R., Thomas, F., Potukuchi, P., Hung, A., & Kovesdy, C. P. (2018). Disparities in Initial Oral Antidiabetic Medication Adherence Among Veterans with Incident Diabetes. Journal of Managed Care & Specialty Pharmacy, 24(4), 379–389. https://doi.org/10.18553/jmcp.2018.24.4.379
Grunberger. (2021, May 18). Should SGLT2 inhibitors be first-line therapy for type 2 diabetes? Yes. It Is Not Right to Put Everyone on Metformin and Wait until It Fails. https://www.healio.com/news/endocrinology/20210507/should-sglt2-inhibitors-be-firstline-therapy-for-type-2-diabetes
Ho, P. M., Bryson, C. L., & Rumsfeld, J. S. (2009). Medication Adherence: Its Importance in Cardiovascular Outcomes. Circulation, 119(23), 3028–3035. https://doi.org/10.1161/CIRCULATIONAHA.108.768986
Huang, C. X., Turk, N., Ettner, S. L., Mangione, C. M., Moin, T., O’Shea, D., Luchs, R., Chan, C., & Duru, O. K. (2022). Does the diabetes health plan have a differential impact on medication adherence among beneficiaries with fewer financial resources? Journal of Managed Care & Specialty Pharmacy, 28(9), 948–957. https://doi.org/10.18553/jmcp.2022.28.9.948
Lee, D. S. U., & Lee, H. (2022). Adherence and persistence rates of major antidiabetic medications: A review. Diabetology & Metabolic Syndrome, 14(1), 12. https://doi.org/10.1186/s13098-022-00785-1
Shin, H., Schneeweiss, S., Glynn, R. J., & Patorno, E. (2022). Evolving channeling in prescribing SGLT ‐2 inhibitors as first‐line treatment for type 2 diabetes. Pharmacoepidemiology and Drug Safety, 31(5), 566–576. https://doi.org/10.1002/pds.5406
Trief, P. M., Kalichman, S., Uschner, D., Tung, M., Drews, K. L., Anderson, B. J., Fette, L. M., Wen, H., Bulger, J. D., & Weinstock, R. S. (2022). Association of psychosocial factors with medication adherence in emerging adults with youth‐onset type 2 diabetes: The i Count study. Pediatric Diabetes, 23(8), 1695–1706. https://doi.org/10.1111/pedi.13431