We recently released insights exploring basketball– and soccer-related sports injuries, which inspired us to look into other sports. With over 15 million baseball players in the US and nearly 70 million people who attended a Major League Baseball (MLB) game in 2019, today – MLB Opening Day, 2023 – we take a look at America’s favorite pastime – baseball and softball (Love, 2019; Statista, 2022).
While in previous sports we’ve seen differences in injuries by sex, in baseball and softball previous research has shown variation in injuries by age groups (Adirim & Cheng, 2003). For younger children playing baseball or softball, being struck by a bat is the most common cause of traumatic brain injuries (TBIs); this differs from older players whose TBI-related injuries are most commonly caused by being hit by a ball (Cusimano & Zhu, 2017). This difference in injury mechanisms made us wonder if there are differences in the percentage of injuries that affect the head and may cause concussions for younger and older individuals playing baseball or softball. Additionally, although baseball and softball have similar rules, we were curious about sex differences in injury profiles (males traditionally play baseball, while females traditionally play softball).
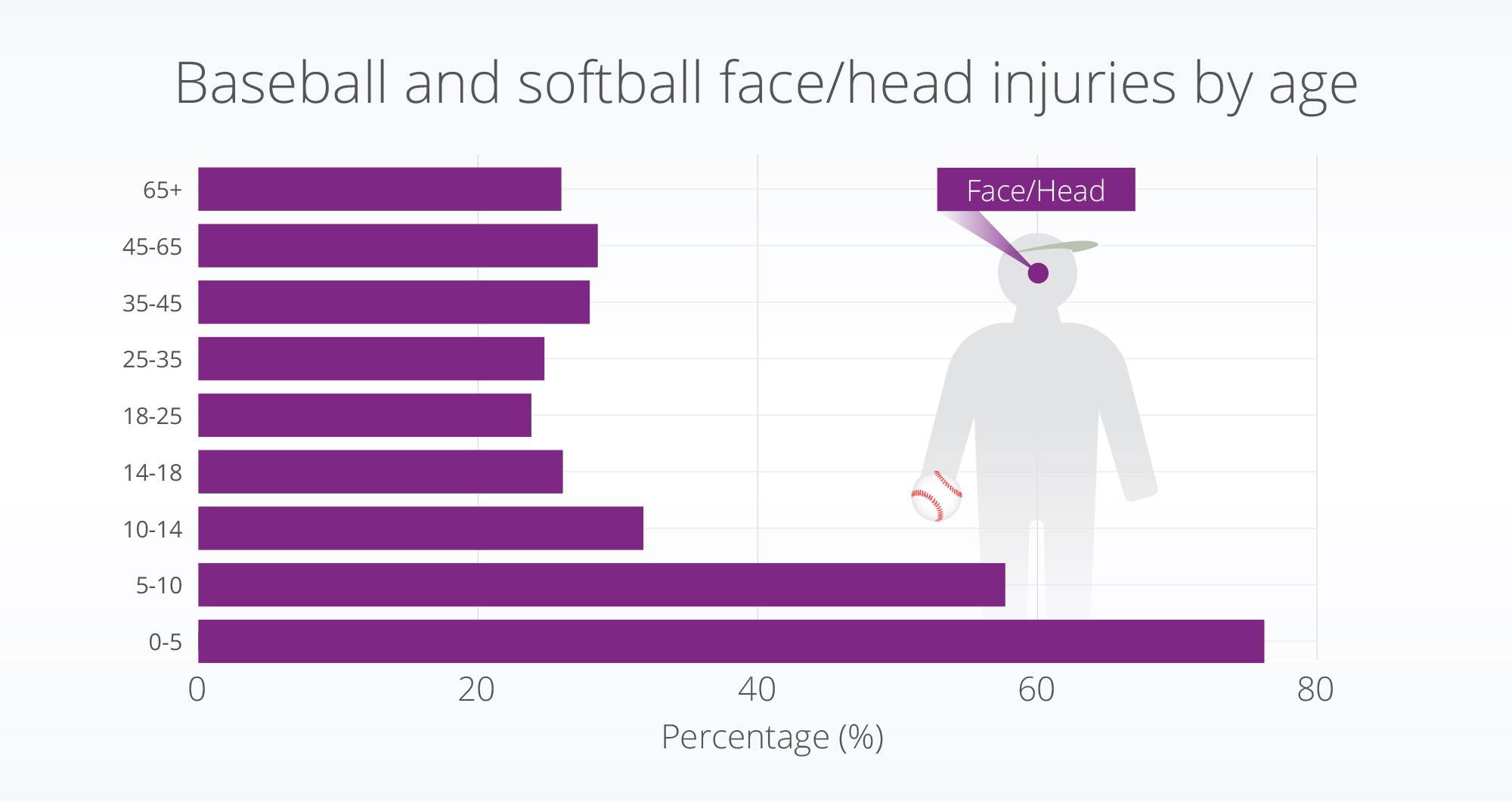
So, what did we find? Within the population who had baseball or softball-related injuries, the youngest age groups in our study (0-5 and 5-10-years-old) had the highest percent of injuries requiring a hospital encounter affecting their head or face. We also did not see large sex differences in the types/rates of injuries which occurred.
Methods
We defined baseball or softball-related injury encounters using a subset of ICD-10 codes. Using a subset of Truveta data, we identified over 16,000 people with over 22,000 baseball or softball-related injury encounters.
We excluded a small set of injuries that were associated with multiple sports. We compared the demographics (age and sex) of those getting injured. We also looked at the location of the encounter to understand when injuries occurred how did people engage with the health care system.
Finally, we classified the body parts that were injured or affected during the baseball or softball injury. We found the diagnostic codes that were associated with the same encounter as the injury and classified them into 13 categories according to injury location (cardiac/chest, concussion/TBI, face/head, groin, lower extremity, neck/back, pain in unspecified location, trunk, upper extremity, other location, unrelated to place of injury on the body). For this analysis, we excluded diagnoses that were classified as ‘other location’ or ‘unrelated to place of injury on the body.’
Results
Who made up the injured population?
It’s important to note that there may be differences between the percentage of people who are engaging in sports and those who are getting injured (Hanson et al., 2005; Harmon et al., 2018).
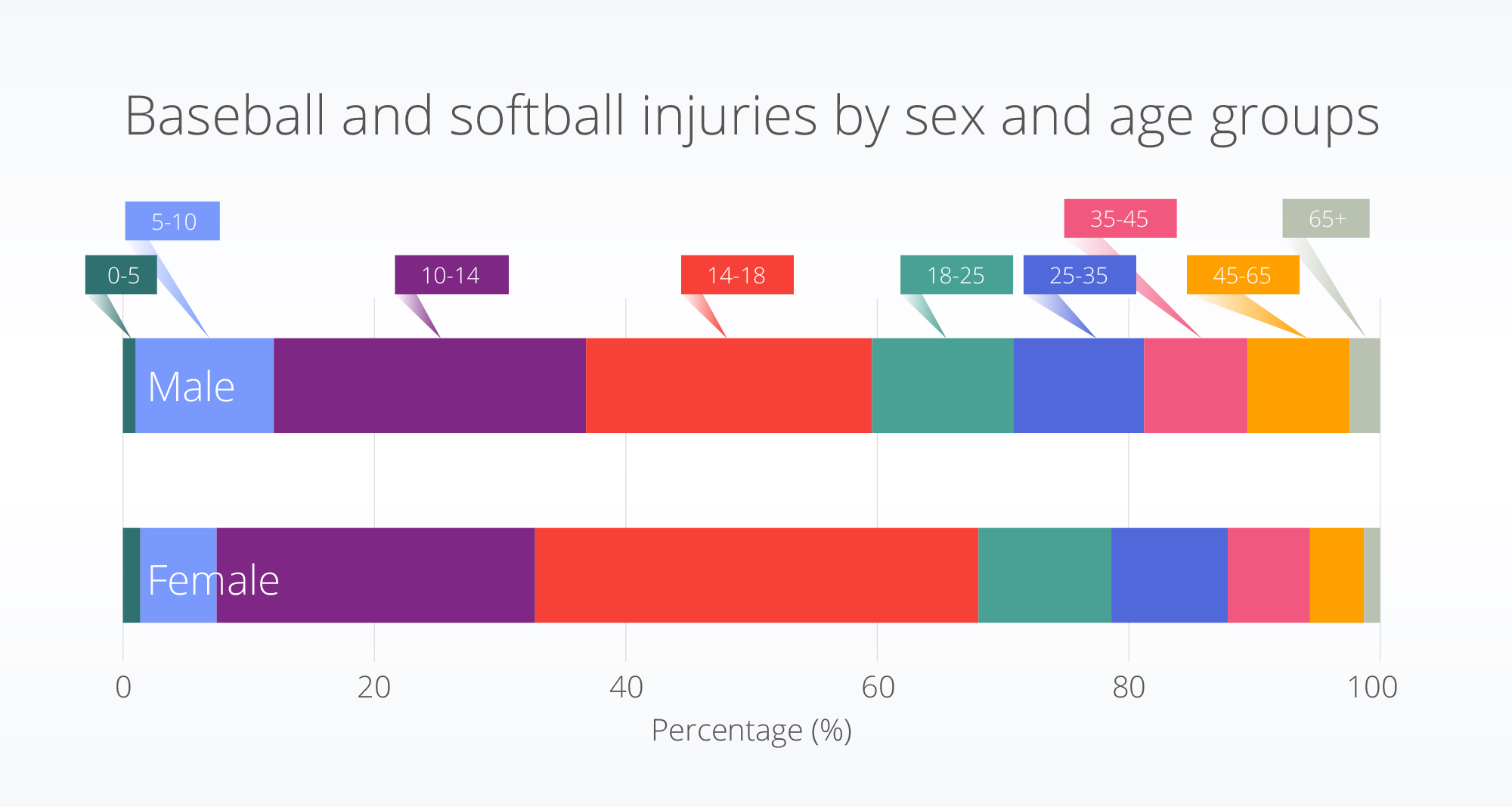
Roughly one-third of the population with baseball or softball injuries were female. More than 50% of the population was between the ages of 10 and 18. A higher percentage (35.3%) of the female injuries occurred in the 14-18 age range compared to the male population within this age range (22.7%).
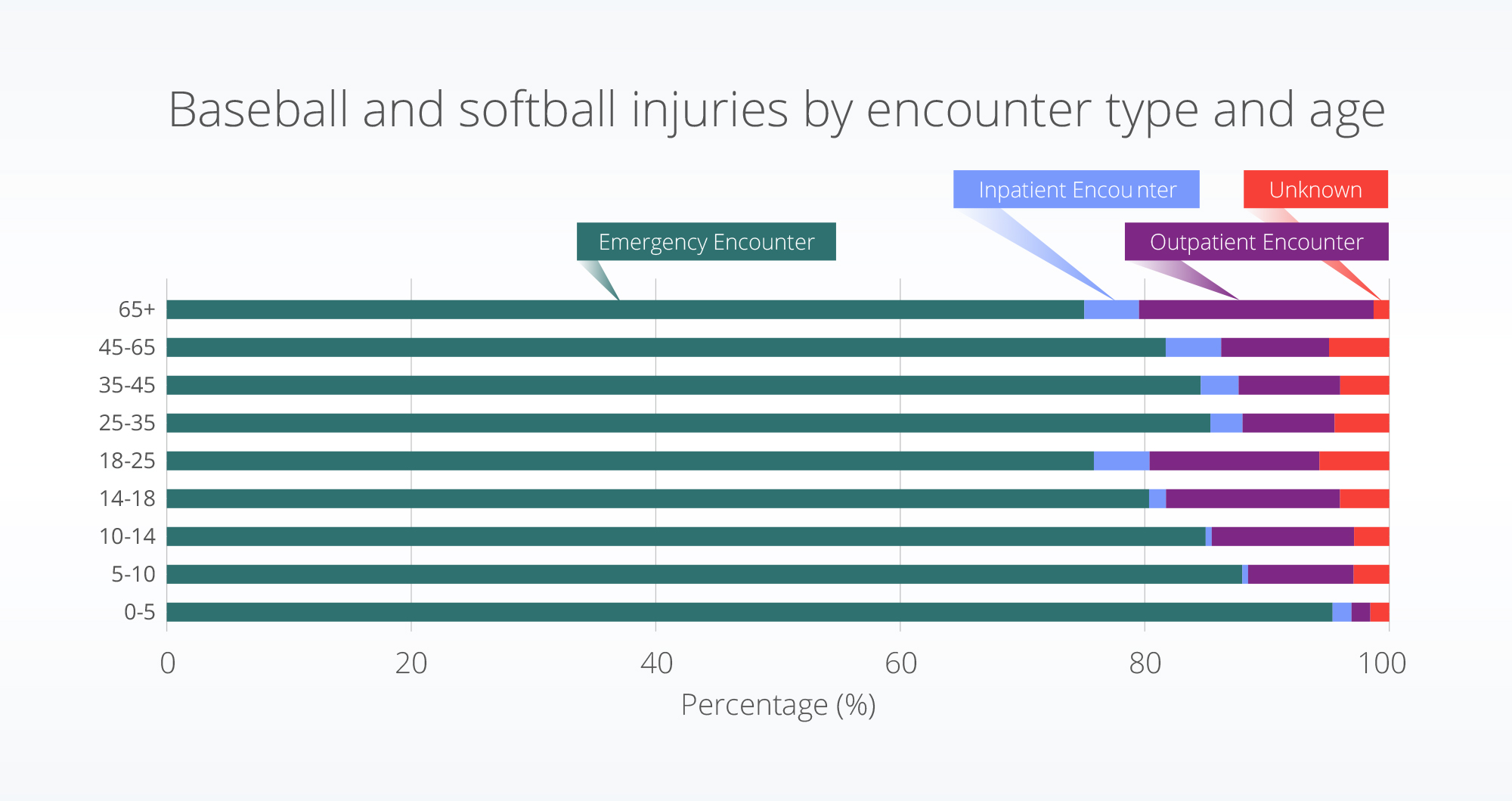
When people had baseball- or softball-related injuries, did they go to the emergency department?
Yes, they did go to the emergency room, especially in the youngest age group (0-5 years old). The percent of inpatient encounters were highest for the 18-25 age group (4.6%), followed up the oldest age groups (45-65 and 65+ years).
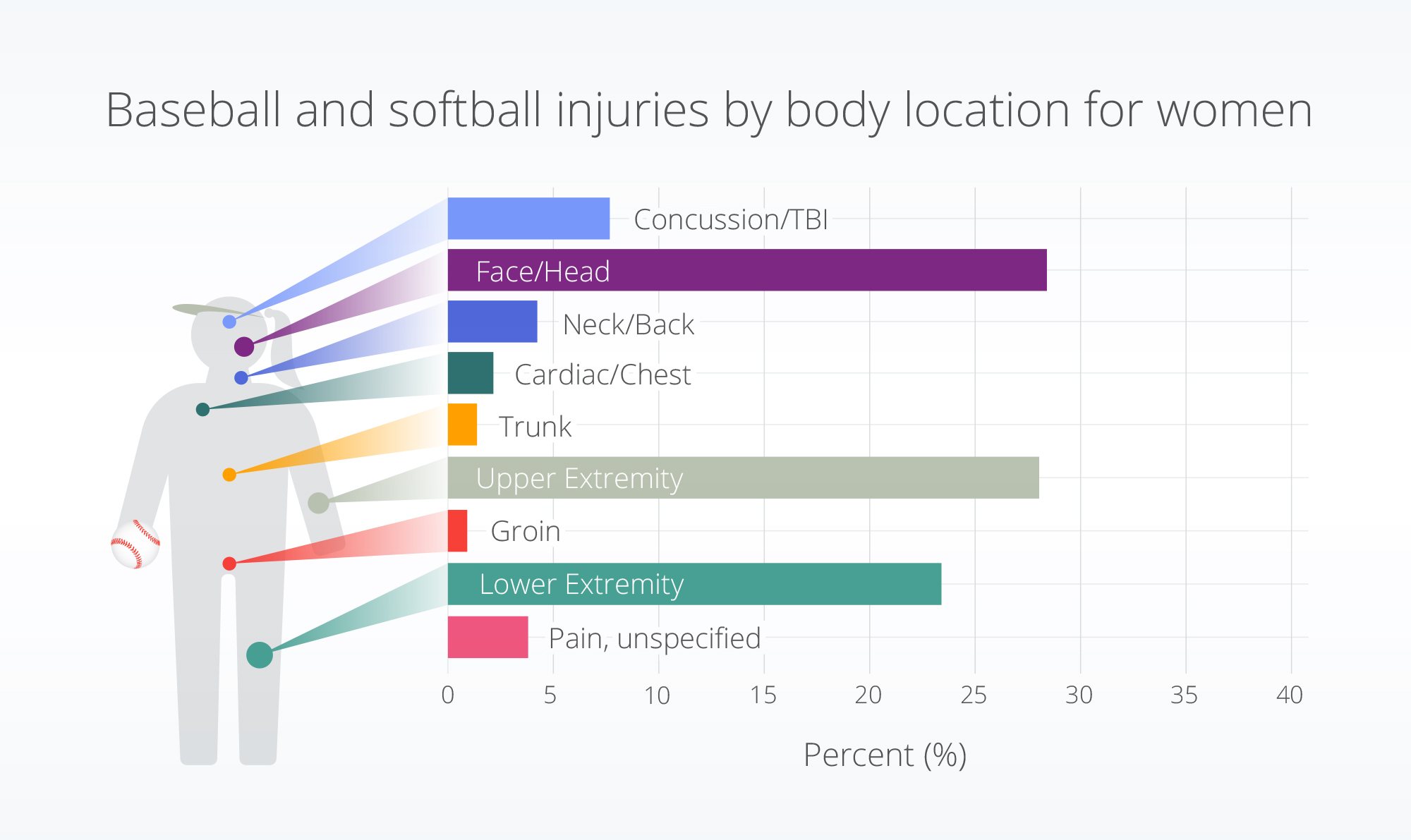
What body part is injured?
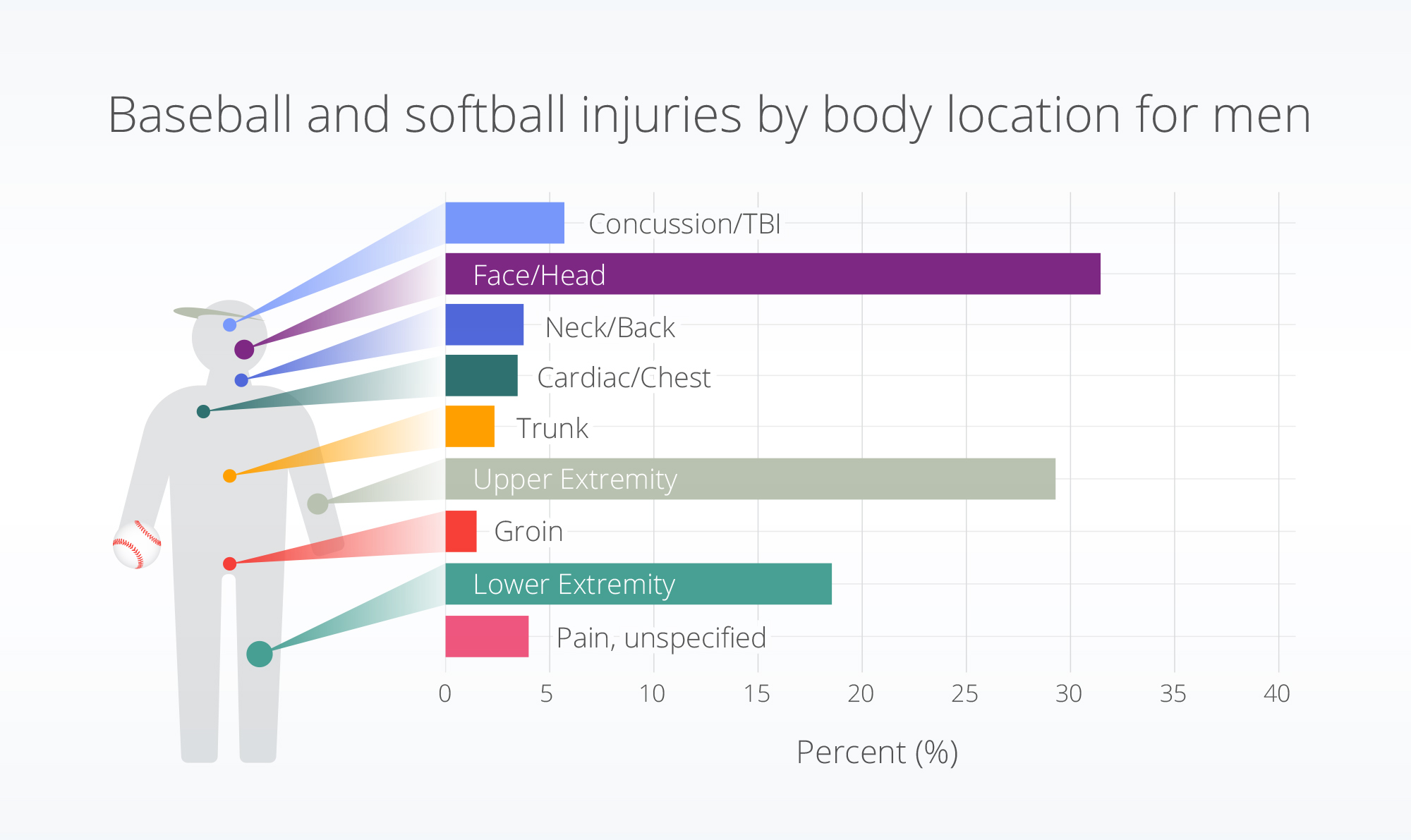
Baseball and softball injuries affected the face and head more than other body parts (30.4% of injuries). The upper extremity had the second-highest rate of injury at 28.9% of injuries.
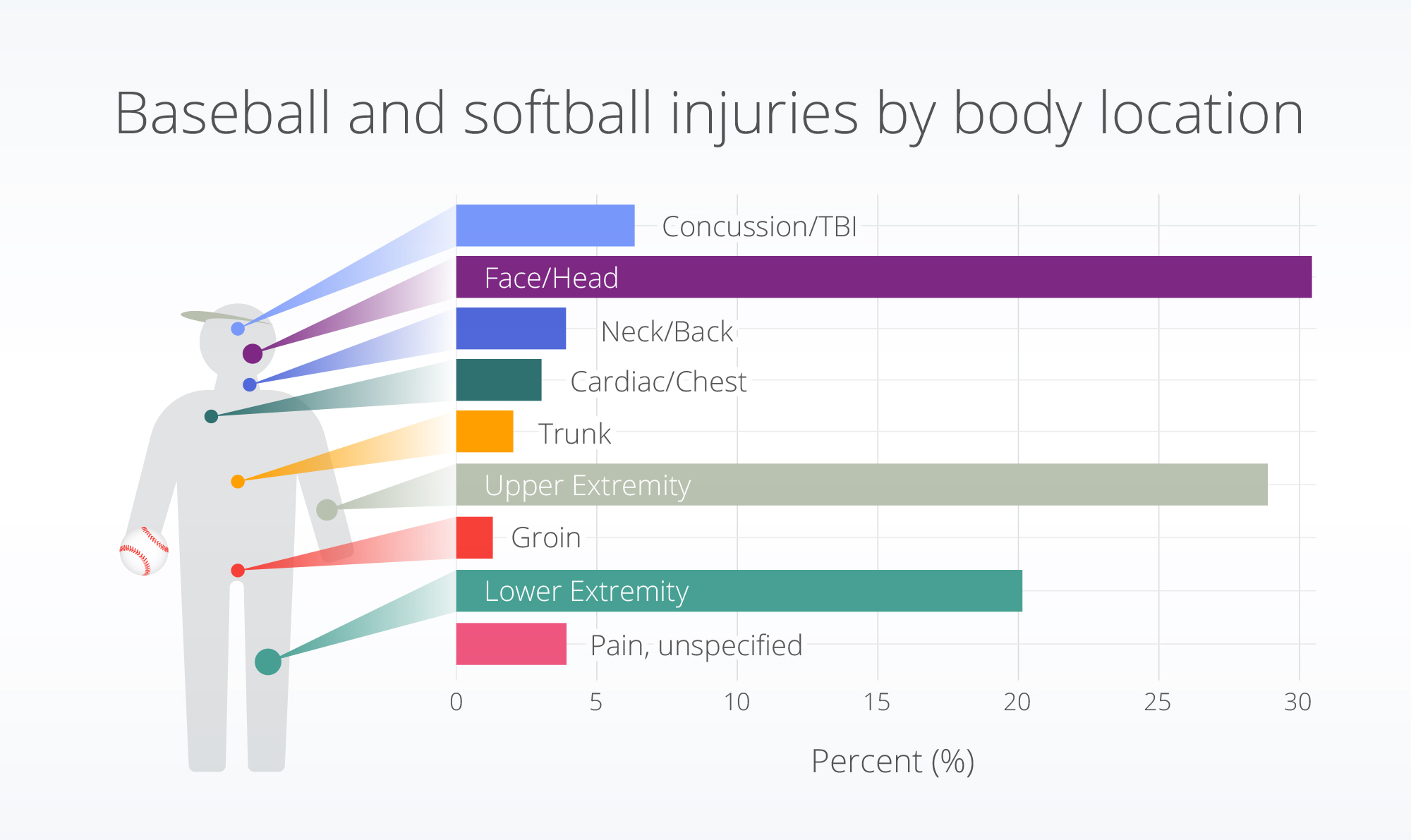
Injury distributions were similar between sexes; however, females who were injured experienced a slightly higher rate of concussions/TBIs (~2% higher) and lower extremity (~5% higher) injuries than males. Males experienced a slightly higher rate of face and head (~3% higher) injuries.
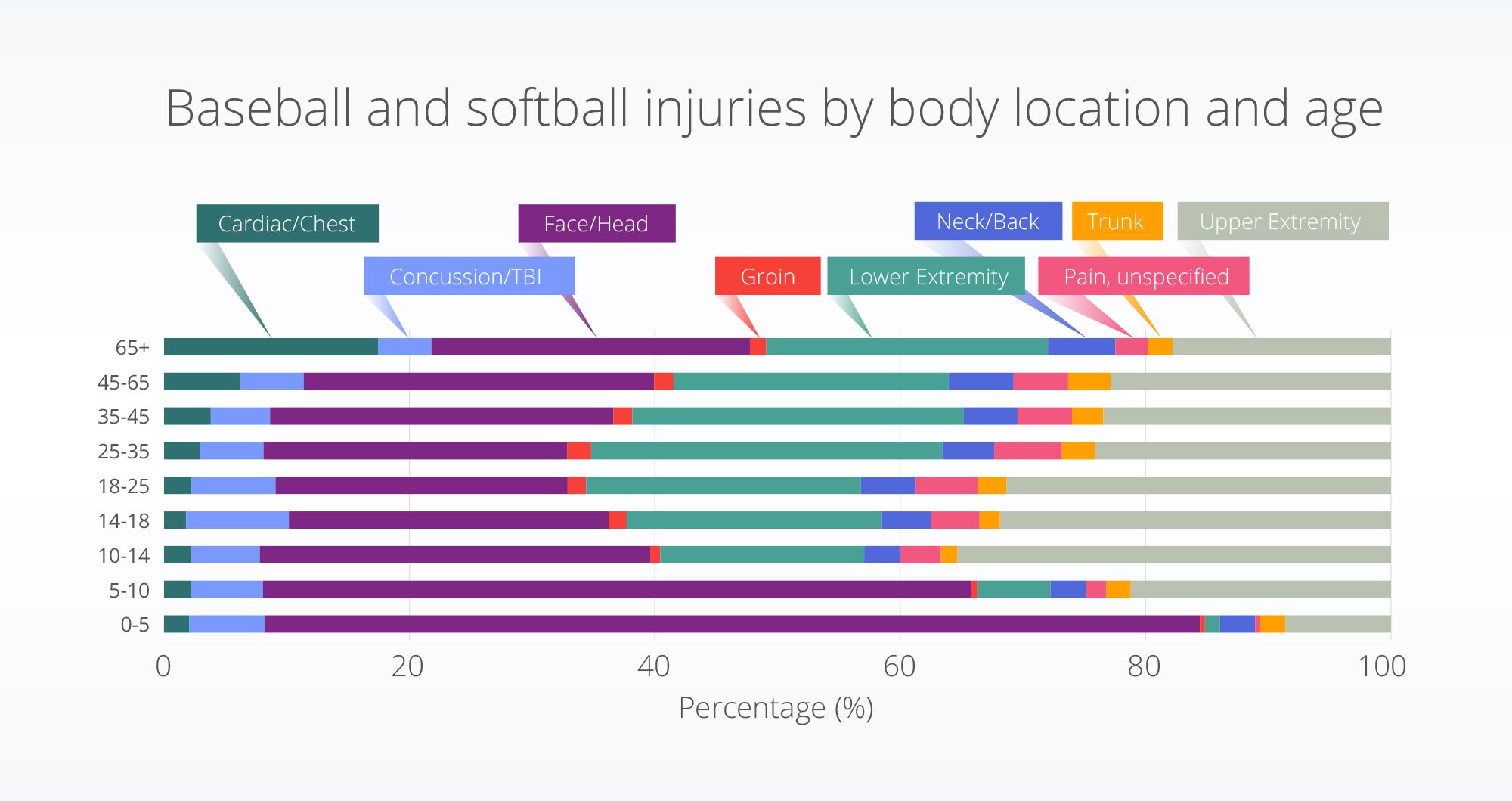
All age groups experienced head and face injuries at a rate over 20% of the total injuries; however, children experienced the highest percent. Of the injuries in the youngest age group (0-5 years old) and the 5-10 age group, over 75% and 50% of injuries, respectively, affected the face and head. The upper extremity was most affected for the 10–14-year-old age group, and concussions were highest for the 14-18 year-olds.
Discussion
Overuse injuries of the upper extremity are very common for high school, collegiate, and professional baseball players (Collins & Comstock, 2008; McFarland & Wasik, 1998; Posner et al., 2011). Although we did not stratify by mechanism of injury (i.e., overuse compared with traumatic), we saw the second-highest percent of injuries in our data to be upper extremity injuries.
In these data we saw the highest percent of injuries to involve the head and face. This may be due to the fact that some overuse injuries may not require a hospital encounter and therefore they are not included in these data. This theory is supported by one report that stated the incidence of softball and baseball injurers were low, and most often minor (Shanley et al., 2011), potentially not resulting in a hospital visit. Although the populations for those aged 0-5 and 5–10-years-old represent a small percentage of the overall injury population, it is of importance that a higher percentage of injuries for this group concerns the face and head. However, it is reassuring that we do not see an increase in the percentage of concussions and TBIs for this age group.
We were intrigued by the high rate of face and head injuries, so we dug further into the associated codes. What we saw most were non-specific codes, such as “unspecified injury of head, initial encounter” and “injury of head.” Future research is needed to dig deeper into the types of face and head injuries and understand their severity and if additional safety protocols might help to prevent them. One report suggests that the primary injury mechanism for younger children acquiring TBIs in baseball and softball is due to athletes being struck by bats (Cusimano & Zhu, 2017). Further research is needed to understand if that same mechanism is at play for the high rate of face and head injuries seen here.
As with any reserach, there are limitations associated with this analysis. First, to be counted as a baseball- or softball-related injury the person had to have an encounter within the hospital. Injuries that did not include a hospital visit would not be captured in our analysis. Further, multiple body parts could be included for one person/injury. To account for this, we counted each body part that was injured but did not look across different injury combinations. Additionally, we classified baseball- or softball-related injuries based on the existence of a subset of ICD-10 codes related to baseball or softball. If a physician did not use these codes, the injury would not be captured within these data. Finally, no statistical analyses were conducted to test for differences between groups or account of the population who was playing baseball or softball. In this study we describe the differences within a population with baseball or softball-related injuries, but additional research is needed to take into account the incidence amongst a population who plays baseball or softball and test for significance.
These data showed more age differences, rather than sex differences in baseball or softball-related sport injuries. In future blogs in this series, we’ll dig deeper into sex differences in injury profiles.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data pulled January 11, 2023.
References
Adirim, T. A., & Cheng, T. L. (2003). Overview of Injuries in the Young Athlete: Sports Medicine, 33(1), 75–81. https://doi.org/10.2165/00007256-200333010-00006
Collins, C. L., & Comstock, R. D. (2008). Epidemiological Features of High School Baseball Injuries in the United States, 2005–2007. Pediatrics, 121(6), 1181–1187. https://doi.org/10.1542/peds.2007-2572
Cusimano, M. D., & Zhu, A. (2017). Systematic Review of Traumatic Brain Injuries in Baseball and Softball: A Framework for Prevention. Frontiers in Neurology, 8, 492. https://doi.org/10.3389/fneur.2017.00492
Hanson, D., Hanson, J., Vardon, P., McFarlane, K., Lloyd, J., Muller, R., & Durrheim, D. (2005). The injury iceberg: An ecological approach to planning sustainable community safety interventions. Health Promotion Journal of Australia, 16(1), 5–10. https://doi.org/10.1071/HE05005
Harmon, K. J., Proescholdbell, S. K., Register-Mihalik, J., Richardson, D. B., Waller, A. E., & Marshall, S. W. (2018). Characteristics of sports and recreation-related emergency department visits among school-age children and youth in North Carolina, 2010–2014. Injury Epidemiology, 5(1), 23. https://doi.org/10.1186/s40621-018-0152-0
Love, J. (2019, October 22). How Popular Is Baseball, Really? https://www.nytimes.com/interactive/2019/10/22/sports/baseball/baseball-popularity-world-series.html
McFarland, E. G., & Wasik, M. (1998). Epidemiology of Collegiate Baseball Injuries. 8(1), 10–13. https://pubmed.ncbi.nlm.nih.gov/9448950/
Posner, M., Cameron, K. L., Wolf, J. M., Belmont, P. J., & Owens, B. D. (2011). Epidemiology of Major League Baseball Injuries. The American Journal of Sports Medicine, 39(8), 1675–1691. https://doi.org/10.1177/0363546511411700
Shanley, E., Rauh, M. J., Michener, L. A., & Ellenbecker, T. S. (2011). Incidence of Injuries in High School Softball and Baseball Players. Journal of Athletic Training, 46(6), 648–654. https://doi.org/10.4085/1062-6050-46.6.648
Statista. (2022, December 8). Number of baseball participants in the United States from 2010 to 2021. https://www.statista.com/statistics/191626/participants-in-baseball-in-the-us-since-2006/
