Peripheral Artery Disease (PAD) is a common disease that causes the arteries in the extremities to narrow. Recently, as part of PAD Awareness Month, we investigated disparities in the frequency of common procedures used to treat PAD, known as endovascular (or minimally-invasive) revascularization. We also investigated the associated outcomes of revascularization, which is used to open the artery and improve blood flow to the areas beyond the narrowed artery. You can read more about what we discovered in the Truveta Research Insights blog.
Truveta also announced a collaboration with Boston Scientific. Their researchers will access Truveta data to gain a deeper understanding of the long-term patient outcomes relating to the use of Boston Scientific’s products indicated for the treatment of peripheral artery disease, as well as other conditions like venous thromboembolic disease and segments of interventional oncology.
In response to the initial PAD research insights we published, we received a question from Michael R. Jaff, DO, Chief Medical Officer, Peripheral Interventions, at Boston Scientific:
“The fact that 6.6% of the PAD population was under 50 is very interesting, since research on this population has been limited. Are you able to dig deeper into this population to understand if there are differences in demographics between the population diagnosed with PAD who are over and under 50 years old?”
Diagnosis of PAD in patients younger than 50 years old is uncommon [1]. As Dr. Jaff indicated, we found that research on the PAD patient population under age 50 is limited, and what does exist often only includes small populations and is often outdated [2]. The limited literature suggests that the diagnosis is commonly missed, and treatment is often under-utilized, so there is an opportunity to increase the recognition and improve the care of those diagnosed with PAD under age 50 [2].
Building on the previous set of insights on the PAD patient population using a subset of Truveta data, we were able to quickly compare the demographics of those diagnosed with PAD who were under age 50 to those who were over age 50.
We found that Black people (inclusive of both Black and African American individuals) make up a higher percentage of the PAD population under age 50 than the PAD population over age 50. We also found similar trends for Hispanic or Latino individuals; Hispanic or Latino individuals make up a larger percentage of the PAD population under age 50 than the PAD population over age 50.
Methods
We used a subset of the Truveta data to identify more than 31,000 patients diagnosed with PAD who are under age 50, as well as more than 425,000 patients diagnosed with PAD who are age 50 and older. We then looked at differences in demographics between the two populations and calculated the percentage of both populations who had a revascularization procedure. We removed patients with missing dates, which we assumed to be invalid.
Results
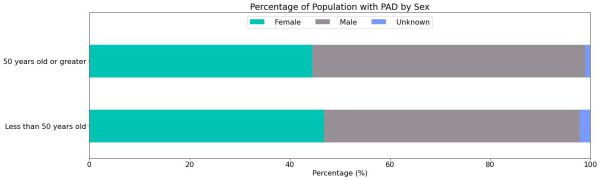
Sex
We found a similar percentage of men and women with PAD in both age groups. The unknowns in this report either indicate the value was not included in the individual’s electronic health record or that it was excluded from the data to protect an individual’s identity as a part of Truveta’s commitment to privacy [3].
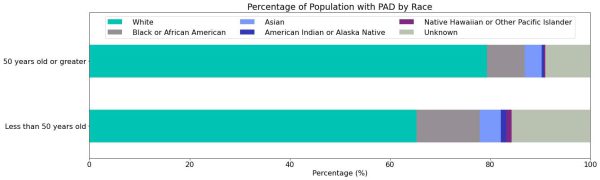
Race
We found sizable racial disparities with Black (12.4%), Asian (4.3%), and American Indian or Alaskan Native (1.1%) groups comprising a higher percentage of the PAD population in the group under 50 years old compared to the older group (7.5%, 3.5%, and 0.3%, respectively).
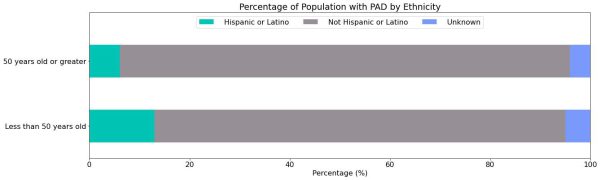
Ethnicity
Importantly, we identified that the prevalence of Hispanic or Latino populations in patients <50 (12.8%) is twice that of the older PAD population (6.1%).
Revascularization
In this population, we see 2.5% of individuals over 50 receive revascularization procedures, while only 1.4% of those under 50 receive revascularization procedures.
Discussion
In the younger PAD group, we see a higher percentage of the population is made up of Black and Hispanic or Latino individuals compared to the older population. This may indicate earlier disease presence and progression in these groups related to the higher incidence of cardiovascular risk factors such as diabetes, obesity, hypertension, and hyperlipidemia in these populations [4]. Ultimately, these risk factors have been shown to be highly influenced by social factors [5].
Our data may also indicate that the prevalence of PAD is underappreciated in patients under 50 years old. In addition, given the challenges in making prompt and accurate diagnoses of PAD in populations older than 50, these data may suggest that the time to diagnosis is even longer, particularly in underrepresented populations. This compounds with the fact that data in the younger PAD population are considered limited [2]. Further research is needed to better understand the population of those with PAD under 50, and supplementing that analysis with social determinant of health data could aid in identifying potential risk factors for those who develop PAD before the age of 50.
As mentioned above, although there is a difference in revascularization rates between the two age groups, this could be due to differences in underlying disease or disease severity for which this study did not control. This study has a few other limitations. First, we looked at unadjusted data; we did not adjust for comorbidities such as diabetes, which have been shown to influence outcomes and are more prevalent in certain populations. Second, while this is a large sample, it does not include all patients in the US; there is a potential for sampling bias where certain groups may be over- or underrepresented (e.g., certain rural regions).
After we completed this follow-up analysis, the Truveta team provided the results to Dr. Jaff. He commented:
“These data are thought-provoking. I am unaware of any modern data which has investigated these disparities and demonstrated these trends, especially for the Hispanic or Latino group. It would be interesting to dig deeper into these data to explore the underlying trends in more detail.”
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data prior to August 25, 2022.
Citations
[1] Mehta, Anurag, et al. “Premature atherosclerotic peripheral artery disease: An underrecognized and undertreated disorder with a rising global prevalence.” Trends in Cardiovascular Medicine 31.6 (2021): 351-358. Premature atherosclerotic peripheral artery disease: An underrecognized and undertreated disorder with a rising global prevalence – ScienceDirect
[2] Soudet, Simon, et al. “Under-Prescription of Medical Treatment for Peripheral Artery Disease in the Under 50s: A Retrospective Study.” Angiology 73.4 (2022): 338-343. Under-Prescription of Medical Treatment for Peripheral Artery Disease in the Under 50s: A Retrospective Study – Simon Soudet, Lorène Bultel, Lamrani Adnane, Thierry Reix, Marie Antoinette Sevestre, 2022 (sagepub.com)
[3] Truveta. Our Approach to Protecting Patient Privacy. Spring 2022. Truveta’s Approach to Patient Privacy.
[4] Kurian, Anita K., and Kathryn M. Cardarelli. “Racial and ethnic differences in cardiovascular disease risk factors: a systematic review.” Ethnicity and Disease 17.1 (2007): 143. https://pubmed.ncbi.nlm.nih.gov/17274224/
[5] Havranek, Edward P., et al. “Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association.” Circulation 132.9 (2015): 873-898. https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000228
