- Aortic stenosis – the narrowing of the valve between the lower left heart chamber (left ventricle) and the aorta – is commonly diagnosed with an echocardiogram and staged according to the disease progression. However, it’s a difficult condition to study across large populations because the echocardiogram results are only captured in clinician notes; however, Truveta Data now include observations from echocardiogram reports.
- In this study, Truveta Research used these echocardiogram data extracted from clinical notes to classify people with aortic stenosis at scale and study aortic stenosis disease progression.
- Of echocardiograms classified as aortic stenosis, the largest group was classified as having mild aortic stenosis (82.7%). Asymptomatic severe or very severe aortic stenosis was classified for 7.2% of echocardiograms, and symptomatic severe or very severe aortic stenosis was classified for 3.0% of the echocardiograms with symptomatic severe high-gradient aortic stenosis, symptomatic severe low-flow, low gradient aortic stenosis with reduced left ventricle ejection fraction, or symptomatic severe low-gradient aortic stenosis with normal left ventricle ejection fraction or paradoxical low-flow severe aortic stenosis.
There are many diseases that can affect the heart, and specifically the valves of the heart. Aortic stenosis is defined as the narrowing of the valve between the lower left heart chamber (the left ventricle) and the aorta and is the most common valve disease to need surgical or percutaneous interventions (Iung, 2003). This narrowing can reduce the amount of oxygen-rich blood leaving the heart. Aortic stenosis can range in severity from mild to severe, and people can experience symptoms as the blood flow decreases (Zimlich, 2024). Symptoms can include heart arrythmias, chest pain, feeling faint or dizzy, shortness of breath, fatigue, and others (Mayo Clinic Staff, 2022).
The prevalence of aortic stenosis increases with age – nearly 30% of people over 65 years of age have some form of aortic stenosis (Pujari & Agasthi, 2023), and up to 9% of people over 75 years of age have severe aortic stenosis (d’Arcy et al., 2016; Pujari & Agasthi, 2023). Although mortality rates are low during asymptomatic phases, there is a dramatic increase in mortality after the onset of symptoms (Généreux et al., 2016; Pellikka et al., 1990; Turina et al., 1987).
Aortic stenosis is commonly diagnosed with an echocardiogram and staged according to the disease progression (Mayo Clinic Staff, 2022). Although the stage of aortic stenosis progression is important for treatment decisions – people with severe or very severe aortic stenosis will receive different treatment than people with mild aortic stenosis – the progression is not typically accessible in traditional EHR or claims data used for clinical research. These data are contained within clinical notes and are not structured like many other data, making them challenging for large-scale cardiovascular research. However, because of the power of clinical expert-led AI, Truveta Data now includes observations from echocardiograms, enabling the study of conditions like aortic stenosis.
For this study, we used these echocardiogram data extracted from clinical notes to classify people with aortic stenosis at scale and study aortic stenosis disease progression. In a subsequent blog, we explore outcomes and disparities among patients with aortic stenosis by severity. The full study — including the classification of severity, patient outcomes, and disparities — is available in Truveta Studio.
Methods
There are five main valve and hemodynamic variables that contribute to aortic stenosis classification: aortic maximum velocity, aortic mean pressure gradient, aortic valve area, left ventricular ejection fraction (LVEF), and aortic stroke volume index. After these data were extracted from clinical notes (using the Truveta Language Model, which makes it possible to extract data from notes), we identified a cohort of people who had an echocardiogram, which included any of the five valve hemodynamic variables.
We conducted additional cleaning steps for each variable.
- Aortic maximum velocity: When units were not available, values between 0-10 were assumed to be meters per second (m/s) and values between 100-1,000 were assumed to be centimeters per second (cm/s) and normalized to all be m/s. This resulted in aortic maximum velocity values between 0-10 m/s.
- Aortic mean pressure gradient: When units were not available, values between 0-120 were assumed to be millimeters of mercury (mmHg). Values over 120mmHg were assumed to be unreasonable, and therefore, all values ranged from 0-120mmHg.
- Aortic valve area: When units were not available, values between 0-5 were assumed to be centimeters squared (cm2), and therefore, all values ranged from 0-5cm2.
- Left ventricular ejection fraction: When units were not available, values between 0-100 were assumed to be a percent, and values between 0-1 were assumed to be a rate and normalized to all be a percent. This resulted in left ventricular ejection fraction values that ranged from 0-100%.
- Aortic stroke volume index: When units were not available, values between 0 -100 were assumed to be milliliter per meter squared (mL/m2), and therefore all values ranged from 0-100mL/m2.
We identified patients with symptoms of heart failure (including both reduced and preserved ejection fraction), chest pain or shortness of breath caused by the heart (angina), and fainting or the feeling that one might faint caused by a drop in blood pressure or heart rate (syncope or presyncope) prior to each echocardiogram. We used each hemodynamic variable in combination with the symptom data to classify eight types of aortic stenosis. People were classified as having symptoms if they had at least one of these prior to the echocardiogram. Aortic stenosis was classified using the 2020 AHA guidelines (Otto et al., 2021):
- Mild progressive aortic stenosis
- Aortic maximum velocity of 2-2.9m/s or aortic mean pressure gradient greater than 20mmHg
- Left ventricle ejection fraction greater than or equal to 50%
- Moderate progressive aortic stenosis
- Aortic maximum velocity of 3-3.9m/s or aortic mean pressure gradient of 20-39mmHg
- Left ventricle ejection fraction greater than or equal to 50%
- Asymptomatic severe aortic stenosis
- Aortic maximum velocity greater than or equal to 4m/s or aortic mean pressure gradient greater than or equal to 40mmHg
- Left ventricle ejection fraction greater than or equal to 50%
- No evidence of symptoms
- Very severe asymptomatic aortic stenosis
- Aortic maximum velocity greater than or equal to 5m/s or aortic mean pressure gradient greater than or equal to 60mmHg
- Left ventricle ejection fraction greater than or equal to 50%
- No evidence of symptoms
- Asymptomatic severe aortic stenosis with left ventricle (LV) systolic dysfunction
- Aortic maximum velocity greater than 4m/s or aortic pressure gradient greater than or equal to 40mmHg
- Left ventricle ejection fraction less than 50%
- No evidence of symptoms
- Symptomatic severe high-gradient aortic stenosis
- Aortic maximum velocity greater than or equal to 4m/s or aortic pressure gradient greater than 40mmHg
- Evidence of symptoms
- Symptomatic severe low-flow, low gradient aortic stenosis with reduced LVEF
- Aortic valve area less than or equal to 1cm2
- Aortic maximum velocity less than 4m/s or aortic pressure gradient less than 40mmHg
- Left ventricle ejection fraction less than 50%
- Evidence of symptoms
- Symptomatic severe low-gradient aortic stenosis with normal LVEF or paradoxical low-flow severe aortic stenosis
- Aortic valve area less than or equal to 1cm2
- Aortic maximum velocity less than 4m/s or aortic pressure gradient less than 40mmHg
- Stroke volume index <35mL/m2
- Left ventricle ejection fraction greater than or equal to 50%
- Evidence of symptoms
The figure below gives a visual of how these data were classified into each aortic stenosis severity category.
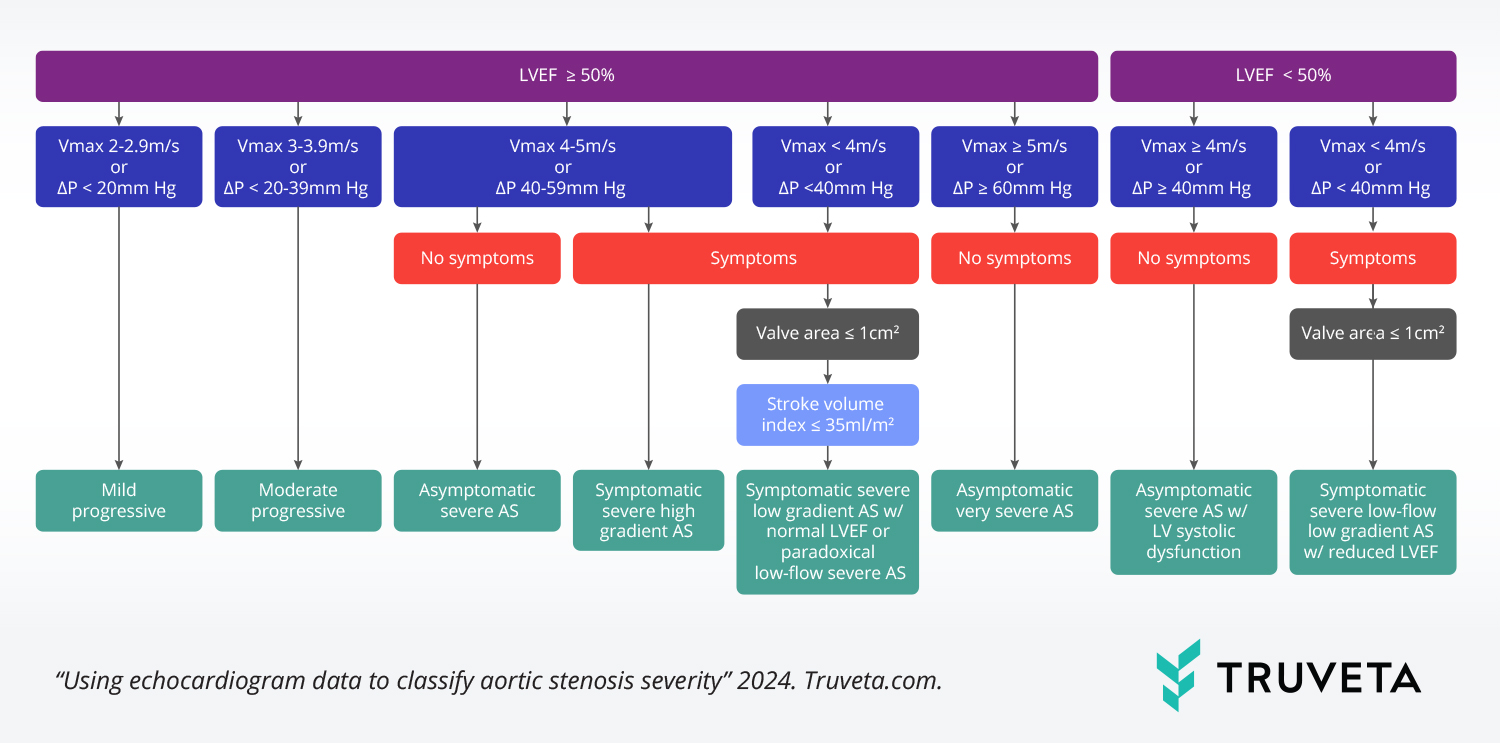
LVEF: left ventricle ejection fraction; Vmax: aortic maximum velocity; ΔP: aortic pressure gradient
Echocardiograms were excluded if severity could not be determined. We quantified the demographic and social drivers of health (SDOH) factors for people with echocardiograms. We also quantified the distributions of aortic stenosis severity, average number of echocardiograms per person, and when more than one echocardiogram existed, the time between the first and last echocardiogram.
Results
Overall population
Using a subset of Truveta Data, we identified more than 1.8 million patients with echocardiograms, with nearly 3 million echocardiograms. The population was primarily female (51.0%), over the age of 65 (50.4%), white (72.6%), and not Hispanic or Latino (79.1%). Nearly half the population was married or in a domestic partnership (49.0%) and made between $35,001 – $65,000 per year (40.3%). The vast majority of the population had a stable place of living within the last year (79.1%) and no record of attending college (81.2%).
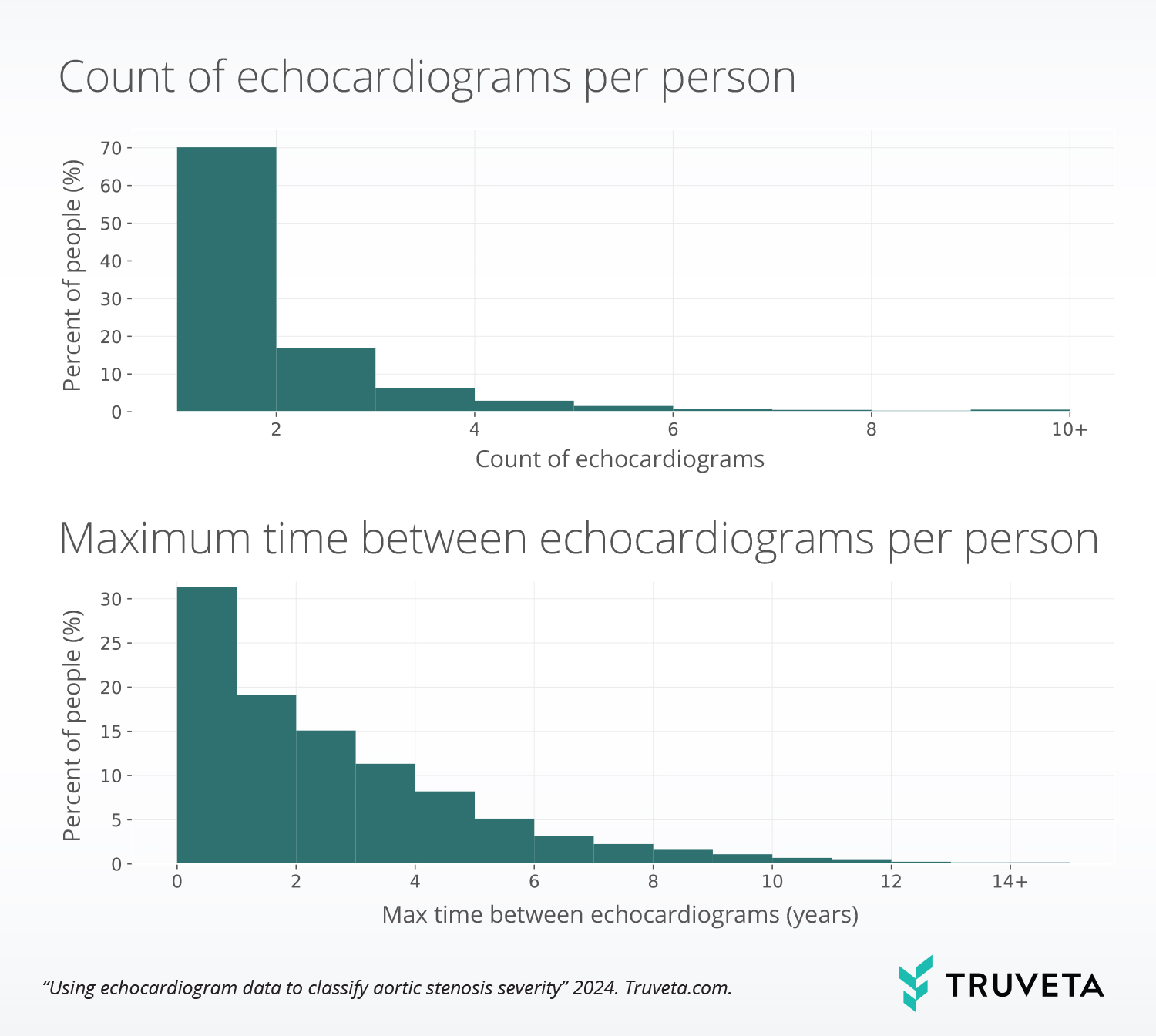
The majority of the population (70.1%) only had one echocardiogram, although 552,039 people had more than one echocardiogram. Within the population who had more than one echocardiogram, over 30% of those echocardiograms happened within one year; however, 23.1% of the echocardiograms occurred four or more years apart.
Aortic stenosis classification
Most echocardiograms were not classified as having a type of aortic stenosis (67.2%). However, based on their hemodynamic values, we found 495,509 people who were classified as having aortic stenosis, and among these patients, there were 971,693 echocardiograms (some of these echocardiograms did not include an aortic stenosis classification).
Of echocardiograms classified as aortic stenosis, the largest group was classified as mild aortic stenosis (82.7%). Asymptomatic severe or very severe aortic stenosis was classified for 7.2% of echocardiograms, and symptomatic severe or very severe aortic stenosis was classified for 3.0% of the echocardiograms with symptomatic severe high-gradient aortic stenosis, symptomatic severe low-flow, low gradient aortic stenosis with reduced left ventricle ejection fraction, or symptomatic severe low-gradient aortic stenosis with normal left ventricle ejection fraction or paradoxical low-flow severe aortic stenosis.
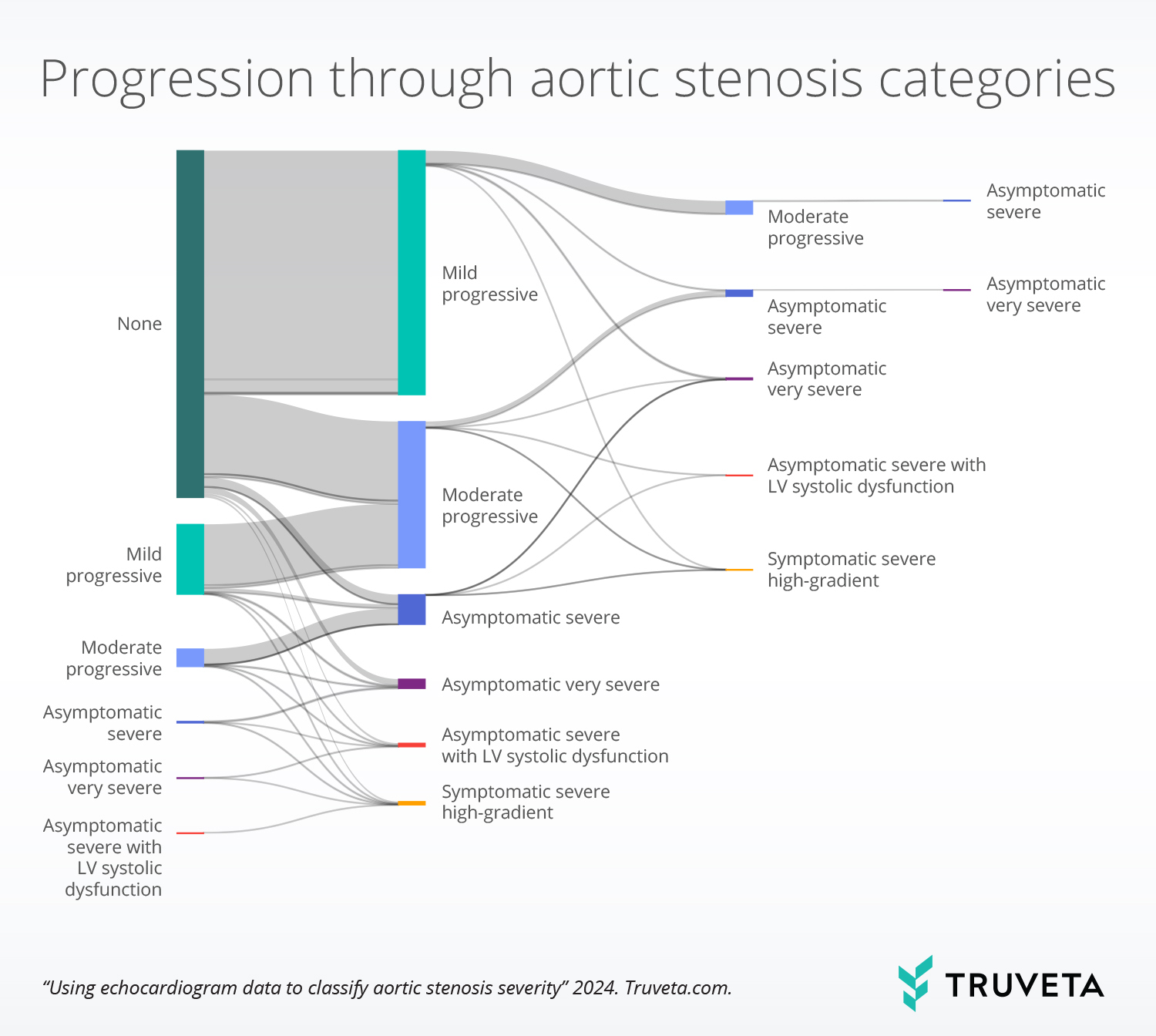
For the population with aortic stenosis and multiple echocardiograms, 22.5% had at least one echocardiogram in which the person did not have aortic stenosis. Within this population, most progress to mild progressive aortic stenosis (70.4%) or moderate progressive aortic stenosis (27.6%) on a subsequent echocardiogram. The plot below shows the distribution of progression through aortic stenosis categories.
We also saw that people spent various lengths of time in each of the aortic stenosis categories. In the figure below, each horizontal line represents one person’s progression through different levels of aortic stenosis severity. This plot also assumes positive progression through each stage and does not take into account if people moved backward in a state or if they had a procedure/treatment that would affect their progression.
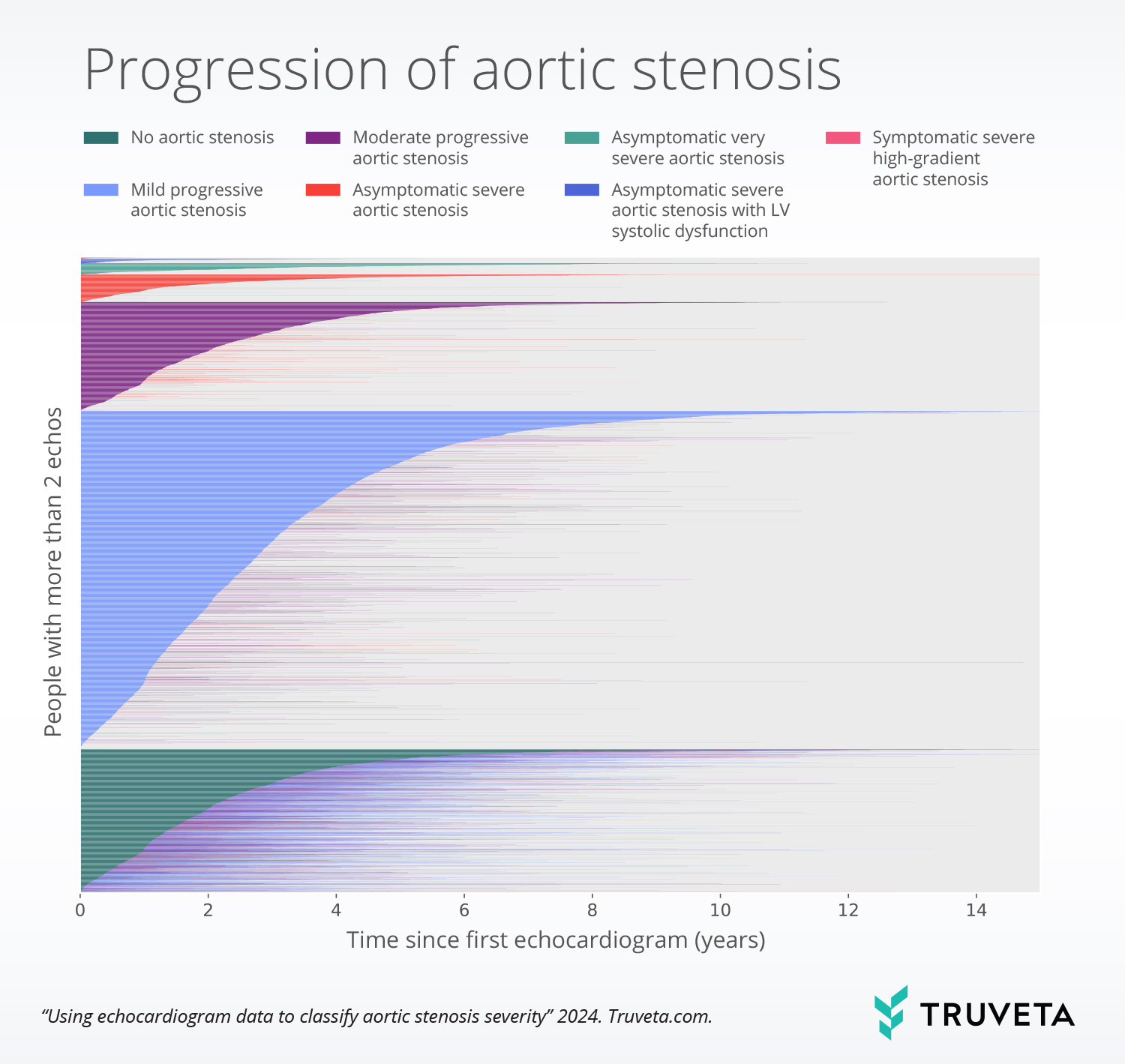
For people who had evidence of only mild progressive aortic stenosis, moderate progressive aortic stenosis, or asymptomatic severe aortic stenosis, there were on average 2.9 ± 2.3, 2.2 ±1.8, and 1.0 ±1.9 years of echocardiogram data, respectively. For people who progressed from no aortic stenosis to mild or moderate progressive aortic stenosis, there was 2.1 years of data without aortic stenosis before progressing to mild or moderate progressive aortic stenosis, where they had 2.3 or 1.7 years of data, respectively.
Discussion
Accessing aortic stenosis severity has traditionally been challenging to capture in EHR or claims data. Using normalized echocardiogram data from Truveta, we were able to classify patients with aortic stenosis by their severity and track their progression over time. For people who were classified as having aortic stenosis and had multiple echocardiograms, most of the population progressed from no aortic stenosis to mild or moderate progressive aortic stenosis. A smaller percentage progressed from having no aortic stenosis to having mild, then moderate, and then severe or very severe. There was also variation in the amount of time people spent in each of these categories.
In this study we used structured echocardiogram data to understand aortic stenosis severity and progression. Structed data provides a foundation for comprehensive analysis and insights into cardiac health. Adding structured echocardiogram data enhances research efficiency, reproducibility, and understanding of longitudinal disease progression and outcomes for cardiovascular research populations. Organized and standardized echocardiogram data enable additional research on large populations that previously may not have been possible at this depth and precision; further advanced analytics, machine learning, and artificial intelligence techniques can be enabled to allow researchers to uncover subtle patterns, predict outcomes, and identify novel biomarkers.
These data highlight the potential questions that can be asked to better understand aortic stenosis progression and outcomes – for example, these data could help answer:
- What demographic factors and comorbidities are associated with aortic stenosis progression?
- Are there pharmacologic treatments that slow progression of aortic stenosis?
- How soon after diagnosis of aortic stenosis do patients receive guideline-based treatment?
- How does aortic stenosis severity and progression influence treatment decisions in at-risk populations, such as the elderly?
- Are there disparities in treatment pathways for people with similar aortic stenosis severity?
- Can we identify patient characteristics and optimal treatment strategies for challenging subpopulations, such as symptomatic severe low-flow, low-gradient aortic stenosis with reduced LVEF?
In the next blog, we explore treatment pathways for people with various aortic stenosis severities. Further, we want to understand if there are disparities in treatments and outcomes for people with similar aortic stenosis disease severities.
The full study — including the classification of severity, patient outcomes, and disparities — is available in Truveta Studio.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on February 13, 2024.
Citations
d’Arcy, J. L., Coffey, S., Loudon, M. A., Kennedy, A., Pearson-Stuttard, J., Birks, J., Frangou, E., Farmer, A. J., Mant, D., Wilson, J., Myerson, S. G., & Prendergast, B. D. (2016). Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: The OxVALVE Population Cohort Study. European Heart Journal, 37(47), 3515–3522. https://doi.org/10.1093/eurheartj/ehw229
Généreux, P., Stone, G. W., O’Gara, P. T., Marquis-Gravel, G., Redfors, B., Giustino, G., Pibarot, P., Bax, J. J., Bonow, R. O., & Leon, M. B. (2016). Natural History, Diagnostic Approaches, and Therapeutic Strategies for Patients With Asymptomatic Severe Aortic Stenosis. Journal of the American College of Cardiology, 67(19), 2263–2288. https://doi.org/10.1016/j.jacc.2016.02.057
Iung, B. (2003). A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. European Heart Journal, 24(13), 1231–1243. https://doi.org/10.1016/S0195-668X(03)00201-X
Mayo Clinic Staff. (2022, August 18). Aortic valve stenosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/symptoms-causes/syc-20353139
Otto, C. M., Nishimura, R. A., Bonow, R. O., Carabello, B. A., Erwin, J. P., Gentile, F., Jneid, H., Krieger, E. V., Mack, M., McLeod, C., O’Gara, P. T., Rigolin, V. H., Sundt, T. M., Thompson, A., & Toly, C. (2021). 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation, 143(5), e72–e227. https://doi.org/10.1161/CIR.0000000000000923
Pellikka, P. A., Nishimura, R. A., Bailey, K. R., & Tajik, A. J. (1990). The natural history of adults with asymptomatic, hemodynamically significant aortic stenosis. Journal of the American College of Cardiology, 15(5), 1012–1017. https://doi.org/10.1016/0735-1097(90)90234-G
Pujari, S. H., & Agasthi, P. (2023). Aortic Stenosis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557628/
Turina, J., Hess, O., Sepulcri, F., & Krayenbuehl, H. P. (1987). Spontaneous course of aortic valve disease. European Heart Journal, 8(5), 471–483. https://doi.org/10.1093/oxfordjournals.eurheartj.a062307
Zimlich, R. (2024, February 12). How Fast Does Aortic Stenosis Progress? Healthline. https://www.healthline.com/health/heart/aortic-stenosis-progression
