At the start of the pandemic, clinicians around the world were struggling for answers. No one knew the best ways to treat patients with COVID-19 infections – when to intubate, which treatments actually work, and more. That’s why more than 20 U.S. health systems have come together to form Truveta, creating the most complete, highest quality, and timely U.S. public health data platform.
As the Truveta Research team, we’re honored to be the first users of the Truveta data. We’ve spent almost a year now digging into Insights and studies to better understand health across our de-identified population with an initial focus on better understanding COVID. The value of Truveta is its completeness, validity, timeliness, and representativeness – all very important factors to ensure valid scientific research. With the rapid pace of a pandemic, we must continuously monitor the safety and effectiveness of vaccines and treatments against these variants. Just as the virus is morphing and evolving into new variants, we are constantly evolving our questions about COVID. As with all research, there are various limitations in the data and methods used. Each detailed blog associated with the Insights below includes a complete view of the methodology and limitations.
Today we take a look back at what we’ve learned so far, and how we’ve been able to use the Truveta platform to ask questions, explore new areas, and share insights to help the community learn as we address this rapidly changing virus.
Understanding COVID infection and hospitalization trends
As a company created out of the pandemic, it seemed only fitting that we began our research journey by focusing on what we could learn about COVID-19 infection rates, hospitalizations, and vaccination trends.
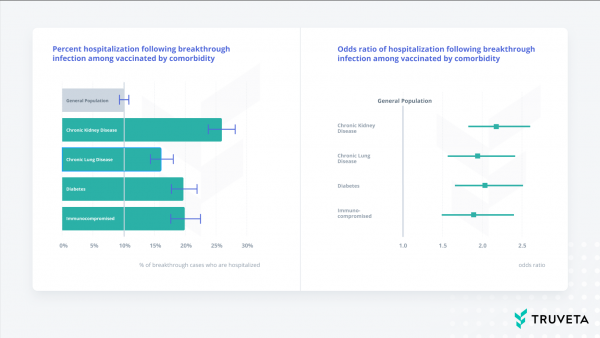
Breakthrough infections and hospitalizations among those with co-morbidities
We shared our first insights in November 2021 when we looked at breakthrough infections and hospitalizations among those who are vaccinated and have co-morbidities. What we found was those patients with co-morbidities – specifically chronic kidney disease (CKD), chronic lung disease, diabetes, or who are immunocompromised – were nearly twice as likely to be hospitalized than the general vaccinated population. At the time, these findings supported the recommendations for patients in these populations to consider booster vaccines, and this paper is available as a pre-print and is undergoing peer review at a reputable scientific journal. Interestingly enough, the CDC published a study two months later on the same topic with remarkably similar results, validating the speed and quality of the data within the Truveta platform.
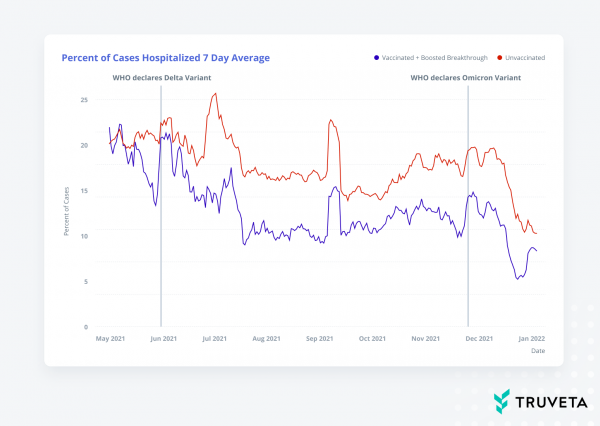
Comparing infection rates and hospitalizations among Delta and Omicron waves
As Delta waned and the Omicron variant emerged and began to dominate infections in the U.S. in January 2022, we then started to explore a comparison between hospitalization and infection rates during Delta and Omicron among unvaccinated, vaccinated, and boosted patients. As we looked at these data, we found that the percentage of people with COVID who were hospitalized was stabilizing and even decreasing with Omicron, and a higher percentage of hospitalizations occurred for unvaccinated patients compared to the vaccinated and boosted population, especially with Omicron.
Then in February and March 2022, we looked at vaccination trends to see which vaccines people were getting as they received their initial vaccinations and booster doses, explored post-COVID infection incidents of heart inflammation in hospitalized patients, and revisited breakthrough infections among those with co-morbidities, but this time during the Omicron wave.
We were excited about how the Truveta platform could enable us to quickly ask new questions about COVID, especially as the virus morphed and public discussions shifted.
Exploring other impacts of the pandemic on daily life
The COVID-19 pandemic affected every aspect of many of our lives. For some, it affected how we work, where we work, who we interact with, and the frequency at which we interact with others.
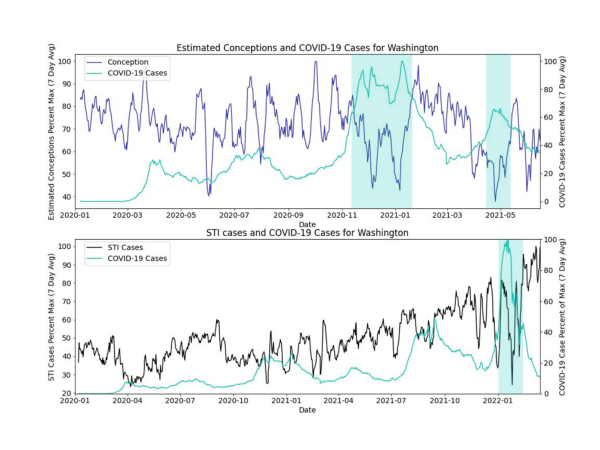
As we thought about the various impacts of social distancing, we were curious if periods of high COVID-19 case rates correlated with decreases in 1) sexually transmitted infections (STIs) and 2) birth rates 9 months later (conception).
What we found was at the state-level in some cases, there appeared to be a decrease in STI and conception rates at time points with COVID-19 peaks, especially later in the pandemic. However, because we didn’t account for seasonality of conception rates or other factors which affect STIs, such as weekdays vs. weekends, there’s more to study.
Learning about long COVID
As we continue to ask new questions about COVID, the pandemic, and discuss ongoing vaccination strategies, a new area of research has emerged: long COVID. Some diagnosed with COVID-19 have a variety of post-COVID-19 symptoms, commonly referred to as long COVID. Symptoms vary and can include cardiovascular, coagulation, and hematologic, gastrointestinal, kidney, mental health, metabolic, musculoskeletal, and neurologic disorders [1]. It’s estimated that 1 in 5 adults experience some long COVID symptoms [2], and as such researchers are actively trying to understand the risk factors and downstream effects.
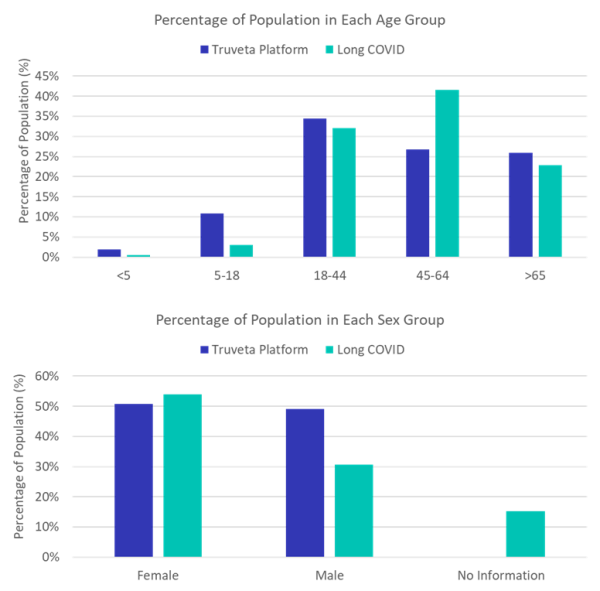
Who is diagnosed with long COVID?
In June 2022, we shared insights about what we were seeing among the population of patients diagnosed with long COVID in the Truveta platform. In our data, we found that females were nearly two times more likely to be diagnosed with long COVID than males.
We also saw that while those aged 45-64 make up 27% of the population in our data, they comprised 42% of long COVID diagnoses, while those 18-44 make up 32% diagnoses and those over 65 years old account for 23% of diagnoses.
Long COVID and mental health
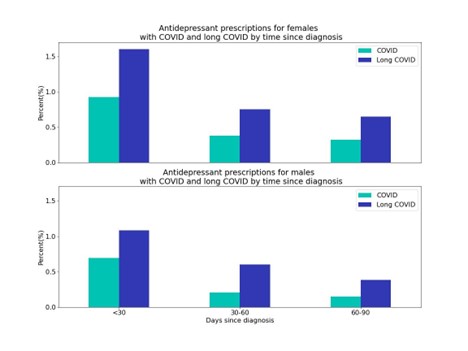
In July 2022, we took a closer look at long COVID to see if there were any possible connections between long COVID diagnoses and mental health in collaboration with Reuters. Looking at a subset of Truveta data, we explored the incidence of a first-time antidepressant prescription within 30, 60, and 90 days of those diagnosed with long COVID. As a comparison, we also looked at trends in first-time prescriptions for those who experienced a first-time COVID infection but were not diagnosed with long COVID.
We found that it’s likely that long COVID not only affects people physically, but also mentally. Adults with long COVID were nearly two times more likely to receive a first-time antidepressant prescription in the first 90 days following a diagnosis (2.6%) than someone with a COVID infection (1.4%). In adolescents (aged 12-17), those diagnosed with long COVID were also nearly two times more likely to receive a first-time antidepressant prescription in the first 90 days following their diagnosis (5.4%) than someone with a COVID infection (2.8%).
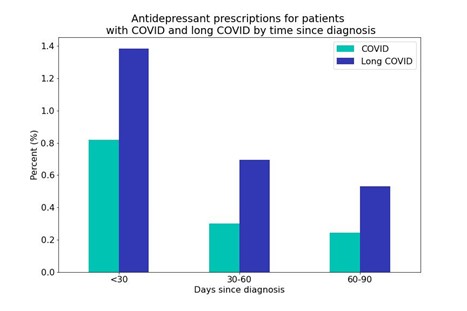
We also found that women were prescribed first-time antidepressants at a higher rate (COVID = 1.6%; long COVID = 3.0%) than men (COVID = 1.1%; long COVID = 2.1%).
For the long COVID population, those aged 18-44 were more likely to get a first-time prescription (3.1%) compared with those 45-64 (2.5%) and over 65 (2.0%) within the first 90-days of the diagnosis.
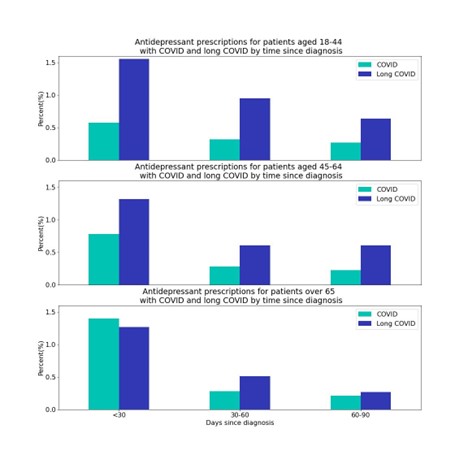
These results emphasize that as clinicians and researchers aim to further understand the complexities related to long COVID, healthcare providers must be acutely aware of their patients’ mental health.
Beyond COVID
While we have focused primarily on research related to COVID, we have also started to explore other trends. For example, Dr. Bapu Jena, a Harvard physician and economist and the host of the Freakonomics MD podcast, reached out to us to learn more about whether the death of actor Chadwick Boseman had an impact on colonoscopy screening rates in African American or Black men in the months following his death (we did not find a correlation).
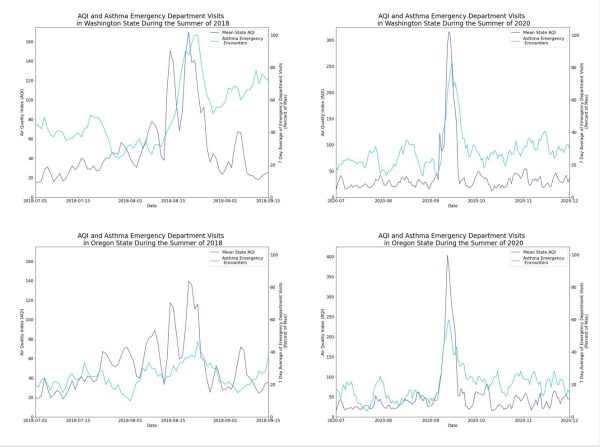
For Earth Day in April 2022, we looked at the impact of air quality on emergency department visits. We explored periods of time in which the air quality index (AQI) peaked in Oregon and Washington (values over 100) to see if there were corresponding peaks in emergency department visits for asthma. We found that when AQI peaked, we also see a peak in ED visits for asthma 1-3 days later, showing a potential connection between high AQI and asthma ED visits. Our health impacts how we interact with the world, as the world around us impacts our health. These data highlight the research opportunity to study the interconnectedness of our health and environment with the use of third-party data to generate new types of insights.
Still so much to learn
Truveta was created with the vision of saving lives with data. Truveta aims to help researchers find cures faster, empower every clinician to become an expert, and help families make the most informed decisions about their care.
All these learnings about COVID and other conditions are just the beginning. We uniquely connect life science and health system researchers to innovate collaboratively, decrease the time from question to insight, and earn trust through transparency and reproducibility of research. We are excited to see what we can learn together.
[1] Al-Aly, Ziyad, Benjamin Bowe, and Yan Xie. “Long COVID after breakthrough SARS-CoV-2 infection.” Nature Medicine (2022): 1-7.
[2] Bull-Otterson L, Baca S, Saydah S, et al. Post–COVID Conditions Among Adult COVID-19 Survivors Aged 18–64 and ≥65 Years — United States, March 2020–November 2021. MMWR Morb Mortal Wkly Rep 2022;71:713–717. DOI: http://dx.doi.org/10.15585/mmwr.mm7121e1.
